Drug consumption and medication cost analysis after spinal cord
advertisement

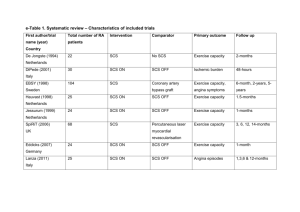
Drug consumption and medication cost analysis after spinal cord stimulation in chronic pain patients Moujahed Labidi, MD PGY-II Neurosurgery Jérome Villeneuve, PhD Sylvine Cottin, PhD Sarah-Maude Caron-Cantin Véronique Briand-Carle Michel Prud’homme, MD PhD Léo Cantin, MD FRCSC Introduction • Chronic neuropathic pain is a frequent clinical entity with reported prevalence of 27 % of patients in pain clinics and up to 8% in the general population (Torrance et al., 2006). It is a debilitating and costly disease (Berger et al., 2004) • In a retrospective review of our cases of spinal cord stimulation for these patients, we demonstrated that 40% mean reduction in pain levels, a significant improvement in quality of life and an 80% satisfaction rate(unpublished data). Introduction • Does SCS reduce medication consumption and drug cost? • The cost-effectiveness of the procedure is established in some indications o CRPS (Kemler et al., 2002) o FBSS (Kumar et al., 2002) (North et al., 2007) • Relatively few data on medication following SCS implantation o North et al. 2005 o Kumar et al. 2008 Methods • Retrospective observational study of all consecutive patients who underwent implantation of a SCS between January 1st, 2000 and June 31st, 2009. o Consent was obtained from all the participants • Baseline characteristics and indication for surgery were obtained from charts. • Medication was assessed with the profiles as effective in the immediate preoperative period and as of July 2009. They were obtained from charts and community pharmacies, respectively. • Morphine equivalents were calculated according to a published equianalgesic tables. Total medication cost was calculated on a price per pill basis, according to our institution’s formulary in July 1st. Patients 131 SCS implantations 77 Exclusions - 54 included patients 23 Data unavailable 20 SCS removed 12 Refusal to participate 8 Invalid data 4 Deceased 3 Non-functioning SCS 2 IT morphine pump Results • There was 21 women (39%) and 33 men (61%) and the mean age at implantation was 50 ± 2 years and 48 ± 2 years for women and men, respectively • The mean duration since surgery was 33 ± 25 months • The most frequent indication was FBSS followed by CRPS Etiology n % FBSS/Chronic radicular pain 30 55.6 CRPS 10 18.5 Multiple sclerosis 2 3.7 Trauma 1 1.9 Peripheral nerve injury 1 1.9 Other neuropathic etiology 8 14.8 N/D 2 3.7 Total 54 100% Results Number of patients Pre SCS Post SCS Percent Pre SCS Post SCS Antiepileptics 26 25 48.15 46.30 Antidepressants 19 21 35.19 38.89 NSAIDs/COX-2 inhibitors/ Salicylate 9 8 16.67 14.81 Benzodiazepines 15 14 27.78 25.93 Hypnotics 1 1 1.85 1.85 Muscles relaxants / Antispasmodics 1 6 1.85 11.11 Opioids 31 33 57.41 61.11 Other analgesics 6 0 11.11 0.00 Results • Opiate consumption *Reduction not associated with preop level of opiates or duration since surgery o Preop : 87 ± 118 mg/d o Postop : 99 ± 172 mg/d • P = 0.29 Difference in opiate consumption following SCS 20 33% 18 16 Increase (33%) Decrease (34%) 14 12 Number of patients 19% 17% 10 8 11% 6 4 6% 7% 7% 101 to 200 >200 2 0 <-200 -200 to -101 -100 to -1 0 Opiate difference 1 to 100 Results Opiate consumption and gender 500 Opiate consumption (mg/d) * 400 300 200 100 0 M F Pre SCS Post SCS Results • Total drug costs o Preop : 181 ± 25 CAD$/m o Postop : 217 ± 25 CAD$/m • P = 0.23 *Reduction associated with lower preop total drug costs (p < 0.05) Difference in drug cost according to gender 160 140 120 100 Drug cost difference (CAD$) 80 * 60 40 20 0 -20 M F Results Correlation between drug cost difference and age among male patients Drug cost difference (CAD$) Age Discussion • No statistically significant reduction in opiate intake or drug consumption habits following SCS implantation • No statistically significant reduction in total drug cost either • However, 67% of patients achieved stabilisation or even reduction of their opiate intake while noting improvement in their pain levels and quality of life Discussion • There may be a different response and evolution between genders o Different threshold and reaction to pain o Higher prevalence of chronic pain among females o Different expectations from surgery • Medication reduction may be harder among patients taking more medication initially • Limitations of the study o o o o Retrospective design Significant number of exclusion (59%) Important variation in duration since implantation of SCS No standardization of confounding parameters and medical management Conclusion • Opiate consumption reduction is hard to achieve following SCS • This may be especially true for female patients • Actively reducing the medication may be possible without increasing pain levels; this should be studied in a prospective fashion in a pain clinic context