Do Spinal Cord Stimulators Work?
advertisement
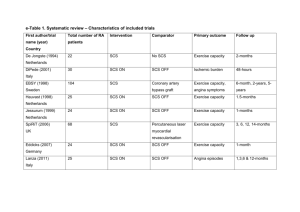
Spinal Cord Stimulator Does It Work? Steve Storick, M.D. Palmetto Health Pain Management and Rehabilitation Center October 15, 2012 Disclaimer • I do not receive any direct compensation from the makers of Spinal Cord Stimulators (Medtronic, St. Jude or Boston Scientific) • I may have stock in all three companies through an investment banker Approved Uses • Chronic Pain of the Trunk or Limbs • Neuropathic Pain – Radiculopathy – Peripheral Neuropathy – Failed Back Surgery Syndrome – Arachnoiditis – Phantom Limb / Stump Pain – Complex Regional Pain Syndrome (RSD) Other Uses • Peripheral Vascular Disease / Ischemic Limbs • Angina Pectoris (not approved in US) Maybe / Maybe Not • • • • • • • • Knee Pain Shoulder Pain Groin / Testicular Pain Mechanical Back Pain Abdominal Pain Post Surgical Pain (Orthopedic) Primarily Back or Neck Pain Many abstracts, but not studies Due Diligence • Extremity Pain • Symptoms c/w neuropathic pain • Test supporting diagnosis – MRI, EMG, Myelogram/CT Scan • • • • Appropriate conservative treatments Surgical remedy? Psychological evaluation SCS Trial Back / Neck Pain • When SCS does not work well • Back or Neck Pain greater than extremity pain • Short term relief during trial and maybe up to 6 months with permanent device • Peripheral Field Electrodes are experimental – Very expensive TENS unit – Placed under skin; not epidural COMPLEX REGIONAL PAIN SYNDROME (CRPS) • • • • • Old term is Reflex Sympathetic Dystrophy (RSD) Usually post traumatic Fracture most common injury Usually affects upper > lower extremity Based on specific subjective and objective criteria (IASP) – 2 0f 4 signs – 3 of 4 symptoms CRPS (RSD) • Patients knowledgeable of symptoms (Internet) but entire clinical picture not c/w CRPS • Chronic pain maybe secondary to surgical trauma • One Physician says so, everyone else does too • No specific test • Incidence 5.5-16.8 per 100,000 Back to SCS Trials • Should have appropriate Psychological Evaluation including testing – Not just a mental status exam • Clear understanding of purpose of SCS and goals (Reduce pain >50-60% and Functional Improvement) • Should last several days • Complications should be unusual • Rarely need repeating Manufacturer • Three Companies (Boston Scientific, Medtronic, St. Jude) • All three equal • Few different bells and whistles • No reason to repeat trial with different system • No reason to replace functioning implanted system w/ different manufacturer CMS proposes 2013 changes • Bundle cost of the lead into 63650 for office • Suggest that L8680 not appropriate code for office setting • Establish values for physician practice expense in the office setting Palmetto GBA Draft (DL32549) • Patients must have undergone careful screening, evaluation and diagnosis by a multidisciplinary team prior to implantation • Must not have active substance abuse issues • Proper patient education about SCS • Appropriate Psychological screening – No major issues including severe depression – May be a candidate if patient receives treatment Palmetto GBA Draft (DL32549) • Can perform SCS trial in office if appropriately supplied and staffed. Must have like privileges in local hospital / ASC or board certified in Pain Management • Preferable that trial physician also implant permanent • Successful trial should be associated w/ at least 50% reduction of target pain or analgesic medication and show some element of functional improvement Palmetto GBA Draft (DL32549) • Physicians w/ low trial to permanent implant ratio (<50%) will be subject to post payment review – May lead to overimplanting of permanent devices • Reimburse for a maximum of 2 leads or 16 contacts for 1 trial per anatomic spinal region per patient per lifetime • Repeat trial only w/ extenuating circumstances L8680 • • • • CMS pays per contact to maximum of 16 +/- $428 x 16 = $6828 Cost: Free(?) to $1200 per electrode (8 contacts) Procedural codes CPT 63650 and 63650-59 are separate fees • BCBS of SC pays invoice for L8680 Decisions • ASC or Hospital costs $6,000-12,000 or more for trial • In office has led to over utilization • Repeat trials w/ different device companies • No proof one is better than other; different whistles and bells • Wrong reason (diagnosis) or patient Advantages/Disadvantages • • • • • • Less medication More control of pain Functional improvement Limited MRI use Potential interaction with Pacemakers/AICDs Electrocautery/Surgery Outcomes • • • • Over 60 studies of varying quality Lumbar fusions 1 or 2 level or even more? Back to work Private Insurance Patients – When can I go back to work? • WC Patients – I cant work! No, the SCS does not make patient worse – Unless major complication such as infection or nerve damage with implantation THANK YOU