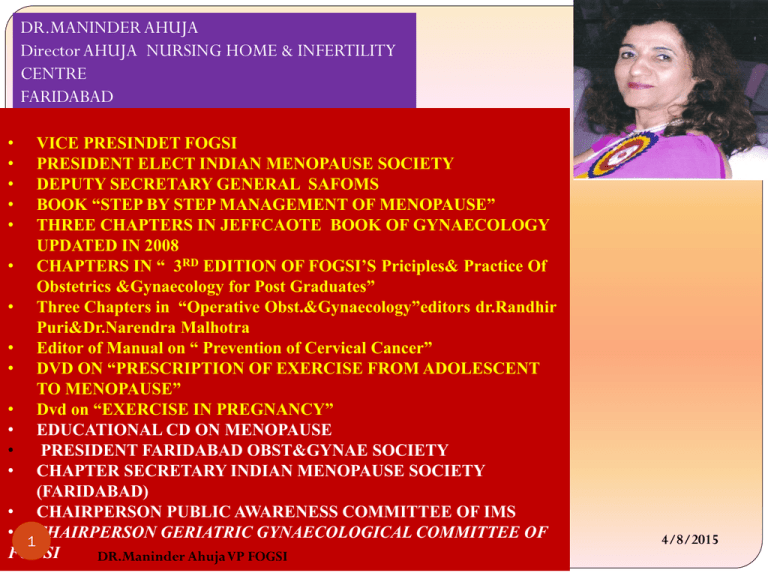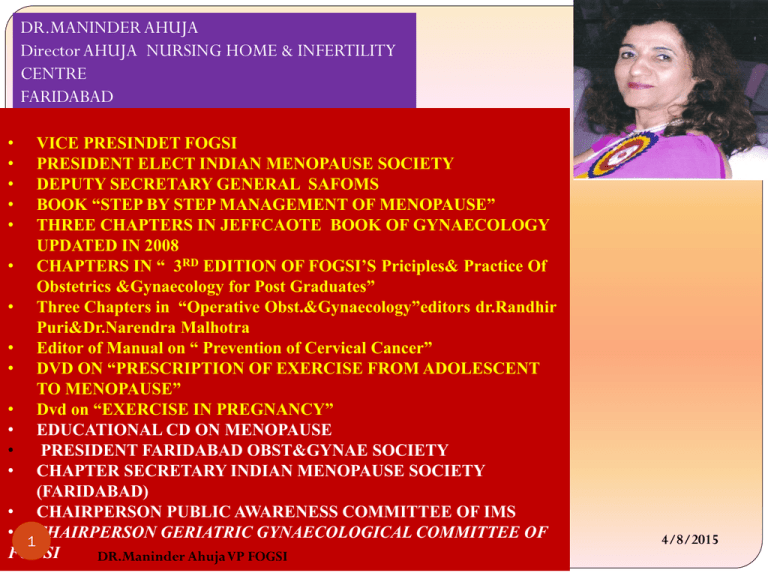
DR.MANINDER AHUJA
Director AHUJA NURSING HOME & INFERTILITY
CENTRE
FARIDABAD
•
•
•
•
•
VICE PRESINDET FOGSI
PRESIDENT ELECT INDIAN MENOPAUSE SOCIETY
DEPUTY SECRETARY GENERAL SAFOMS
BOOK “STEP BY STEP MANAGEMENT OF MENOPAUSE”
THREE CHAPTERS IN JEFFCAOTE BOOK OF GYNAECOLOGY
UPDATED IN 2008
• CHAPTERS IN “ 3RD EDITION OF FOGSI’S Priciples& Practice Of
Obstetrics &Gynaecology for Post Graduates”
• Three Chapters in “Operative Obst.&Gynaecology”editors dr.Randhir
Puri&Dr.Narendra Malhotra
• Editor of Manual on “ Prevention of Cervical Cancer”
• DVD ON “PRESCRIPTION OF EXERCISE FROM ADOLESCENT
TO MENOPAUSE”
• Dvd on “EXERCISE IN PREGNANCY”
• EDUCATIONAL CD ON MENOPAUSE
•
PRESIDENT FARIDABAD OBST&GYNAE SOCIETY
• CHAPTER SECRETARY INDIAN MENOPAUSE SOCIETY
(FARIDABAD)
• CHAIRPERSON PUBLIC AWARENESS COMMITTEE OF IMS
• 1CHAIRPERSON GERIATRIC GYNAECOLOGICAL COMMITTEE OF
FOGSI
DR.Maninder Ahuja VP FOGSI
4/8/2015
DVDs ON
EXERCISE
2
DR.Maninder Ahuja VP FOGSI
4/8/2015
North Zone
Yuva FOGSI
2 0 1 3
Mid life
New Beginnings
22nd Nov to 24th Nov
Venue- Hotel Radisson Amritsar
3
DR.Maninder Ahuja VP FOGSI
4/8/2015
4
DR.Maninder Ahuja VP FOGSI
4/8/2015
SCREENING TESTS PRERUISITES
The ultimate proof of success of cervical screening is its
ability to reduce the incidence of and deaths from cervical
cancer in a cost-effective manner.
One of the prerequisites for effective screening is the
availability of a suitable cervical screening test that has
adequate sensitivity and specificity for detection of
precancerous lesions and that yields reproducible results.
Such a test should be cheap, simple, and easy to apply;
without side effects or complications; as painless as possible;
and socio culturally acceptable.
5
R. Sankaranarayanana,T, L. Gaffikin , M. Jacobc , J. Sellorsd , S. Roblese
a International Agency for Research on Cancer (IARC), 150 cours Albert Thomas, 69372 Lyon
Cedex 08, France b JHPIEGO, Baltimore, MD, USAcEngenderHealth, New York, NY, USA dPATH
(Program for Appropriate Technology in Health), Seattle, WA, USA e PAHO (Pan American Health
Organization), Washington, DC, USA
DR.Maninder Ahuja VP FOGSI
4/8/2015
EARLY DIAGNOSIS AND MANAGEMENT OF
PRECANCEROUS LESIONS IS GOING TO SAVE
MANY LIVES!
Every seven min one woman is dying
of cervical cancer in India.
6
DR.Maninder Ahuja VP FOGSI
4/8/2015
Mother and daughter dyad
7
Every
seven minute one mother is dying of Cervical cancer
!
DR.Maninder Ahuja VP FOGSI
4/8/2015
Cervical cancer screening –Indian
perspective
India is a diverse country with varied scenarios
A uniform strategy can not be implemented
75% of population is in rural or low resource setting
25% of population is in urban high resource setting
Any new program needs to be integrated in the existing
healthcare services
AOGIN guidelines
8
DR.Maninder Ahuja VP FOGSI
4/8/2015
Spectrum of Changes in Cervical Squamous Epithelium
Caused by HPV Infection1
Normal
Cervix
HPV Infection /
CIN* 1
CIN 2 / CIN 3 /
Cervical Cancer
*CIN = cervical intraepithelial neoplasia
9
DR.Maninder Ahuja VP FOGSI
4/8/2015
1. Adapted from Goodman A, Wilbur DC. N Engl J Med. 2003;349:1555–1564. Copyright © 2003 Massachusetts Medical Society. All rights reserved. Adapted with permission.
FOR DEVELOPMENT OF
PRECANCEROUS LESIONS OF CX
We need infection with HPV
Persistence of virus
Leads to precancerous lesions
If they don’t clear then invasive cancer
There is no viremia of natural infection
It is only from local tissue changes that we can diagnose
premalignant lesions
So screening involves exfoliated cells from TZ, from
endocervical glands, and HPV DNA Presenct in tissue
10
DR.Maninder Ahuja VP FOGSI
4/8/2015
11
DR.Maninder Ahuja VP FOGSI
4/8/2015
Screening methods available
VISUAL INSPECTION: VIA and VILLI (subjective visual
inspection with acetic acid &lugol’s iodine
Cytology : Pap Smear, LBC (Liquid based cytology)
HPV DNA Test: High Risk HPV DNA Test / HPV Typing
Follow up with colposcopy or directed biopsy or treat
with ablative methods or excisional methods
12
DR.Maninder Ahuja VP FOGSI
4/8/2015
When to start screening?
Till What Age?
13
DR.Maninder Ahuja VP FOGSI
4/8/2015
MARCH 14 2012 Recommendations for Cx. Cancer screening
Modified from CA Cancer J Clin. 2012;62:147-172 .
Population†
USPSTF ( us preventive task force)
ACS/ASCCP/ASCP( ameirican cancer
Younger than 21 years
Recommends against screening.
Grade: D recommendation.
Women should not be screened
regardless of the age of sexual
initiation or other risk factors.?
21–29 years
Recommends screening with
cytology every 3 years.
Grade: A recommendation.
Screening with cytology alone every 3
years is recommended.
30–65 years
Recommends screening with
cytology every 3 years or for
women who want to lengthen the
screening interval, screening with a
combination of cytology and HPV
testing every 5 years.
Grade: A recommendation.
Screening with cytology and HPV
testing (“co-testing”) every 5 years
(preferred) or cytology alone every 3
years (acceptable) is recommended.
HPV vaccinated
Women who have been vaccinated
should continue to be screened.
Recommended screening practices
should not change on the basis of
HPV vaccination status.
14
DR.Maninder Ahuja VP FOGSI
society, american socieity of colposcopy and
cervical pathology, american society for
clinical pathology)
4/8/2015
Older than 65 years
Recommends against
screening women who have
had adequate prior
screening¶ and are not
otherwise at high risk for
cervical cancer. Grade: D
recommendation.
After hysterectomy
Recommends against
screening in women who have
had a hysterectomy with
removal of the cervix and who
do not have a history of a
high-grade precancerous
lesion (ie, CIN 2 or 3) or
cervical cancer.
Grade: D recommendation
Women with evidence of
adequate negative prior
screening¶ and no history of
CIN2+ within the last 20 years
should not be screened.
Screening should not be
resumed for any reason, even if
a woman reports having a new
sexual partner.
Women of any age following a
hysterectomy with removal of
the cervix who have no history
of CIN2+ should not be screened
for vaginal cancer. Evidence of
adequate negative prior
screening is not required.
Screening should not be
resumed for any reason,
including if a woman reports
having
a new sexual partner.
high-risk populations who may need more intensive or alternative
screenin.
15
These special populations include women 1) with a history of cervical cancer, 2) who were
exposed in utero to diethylstilbestrol (DES), and 3) who are immune-compromised (eg,
infection with human immunodeficiency virus).
4/8/2015
DR.Maninder Ahuja VP FOGSI
WHO Guidelines for screening
cancer cervix
•New programmes should start screening women aged 30 years or more,
and include younger women only when the highest-risk group has been
covered.
•Existing organized programmes should not include women less than 25
years of age in their target populations.
•If a woman can be screened only once in her lifetime, the best age is
between 35 and 45 years.
contd……
16
DR.Maninder Ahuja VP FOGSI
4/8/2015
Contd….
•For women over 50 years, a five-year screening
interval is appropriate.
• In the age group 25-49 years, a three-year interval
can be considered if resources are available.
•Annual screening is not recommended
at any age.
• Screening is not necessary for women over 65 years,
provided the last two previous smears were negative.
17
DR.Maninder Ahuja VP FOGSI
4/8/2015
18
DR.Maninder Ahuja VP FOGSI
4/8/2015
What is critical for Pap smear:
•Accurate sampling.
•Adequate preservation.
•Complete evaluation.
•Meaningful interpretation.
19
DR.Maninder Ahuja VP FOGSI
4/8/2015
WHEN?
8th – 12th DAY OF MC
CERVICAL MUCUS IS ABUNDANT
EXT. OS IS WIDE OPEN
NO RECENT CERVICAL EXAM. / EXPLORATION
/ NO VAGINAL EXAM. WITH A LUBRICANT.
20
DR.Maninder Ahuja VP FOGSI
4/8/2015
Instruments and Materials Required
Sterile Cusco’s speculum
Good light source
Pair of gloves
Ayre’s spatula / endocervical brush
Glass Slides / pencil
Coplin’s Jar
95% ethly alcohol
Cytology form
21
DR.Maninder Ahuja VP FOGSI
4/8/2015
collection devices
Plastic or wooden Ayre’s spatula
Cervix brush
Plastic broom
Ordinary wooden tongue blade
Cotton swab not to be used
22
DR.Maninder Ahuja VP FOGSI
4/8/2015
SAMPLING DEVICES
23
DR.Maninder Ahuja VP FOGSI
4/8/2015
CUSCO’S SPECULUM AND CERVICAL
BIOPSY FORCEP
24
DR.Maninder Ahuja VP FOGSI
4/8/2015
25
DR.Maninder Ahuja VP FOGSI
4/8/2015
How to take a Conventional pap Smear
•
•
•
•
•
•
4/8/2015
Cervix is visualized using a Cusco’s
speculum
Obscuring elements like blood or
mucus is gently removed
The long arm of the spatula or mid part
of the brush is inserted into the
cervical canal and is gently rotated
360o so that the entire TZ is sampled.
The device is removed and the material
obtained is immediately transferred
onto a numbered glass slide taking
care to cover 75% of the surface area
and on one side only.
The slide is immediately put into a
coplin jar containing the fixative 95%
ethanol. Alternatively use spray
fixative at a distance of 12 inches, to
avoid disrupting the cells.
Fixation time: Atleast 30 minutes.
DR.Maninder Ahuja VP FOGSI
27
No.
No.
28
Option 1
DR.Maninder Ahuja VP FOGSI
Option 2
No.
Option 3
4/8/2015
It is better to have two slides
one with brush and one with
spatula
29
DR.Maninder Ahuja VP FOGSI
4/8/2015
Preservative
95% ethinyl Alcohol or 80% Isopropanol
30
DR.Maninder Ahuja VP FOGSI
4/8/2015
Collection of Liquid based Cytology Samples
The cervex brush is used to
collect the sample and the
manufacturer’s instructions are
to be followed.Rotated 5-9times
Central bristles inserted into
cervical canal and lateral
bristles fully bend against
Ectocervix
No smear needs to be prepared
and the entire sample collected
by the brush is transported to
the laboratory in the fixative
vial after proper labelling
4/8/2015
DR.Maninder Ahuja VP FOGSI
31
SAMPLE COLLECTION PROCEDURE – LIQUID BASED CYTOLOGY
32
DR.Maninder Ahuja VP FOGSI
4/8/2015
SAMPLE COLLECTION - HPV HR HYBRID CAPTURE 2
33
DR.Maninder Ahuja VP FOGSI
4/8/2015
What is TZ
34
DR.Maninder Ahuja VP FOGSI
4/8/2015
Comparison Of LBC and PAP
CONVENTIONAL SMEAR LIQUID BASED SMEAR
Heterogeneous
Homogeneous
Graphic cell localization Random cell presentation
300-500 k cells/slide
50-70 k cells/slide
Variable fixation
Thick uneven groups
Uniform fixation
Uniform thin layer
need frequent focusing Not single cell monolayers
Dirty background
Clean background
Variable preservation
Well preserved cells
35
DR.Maninder Ahuja VP FOGSI
4/8/2015
Correlation between different terminologies
Dysplasia
terminology(reagar,1953)
Original CIN
terminology(richart,1968)
TBS(SIL)
terminology,1991
Modified CIN terminology
normal
normal
With in normal
limis.
Benign cellular
changes
normal
Atypia
Koilocytic atypia,flat ASCUS/AGUS/LSIL
condyloma without
epithelial changes
Low grade CIN
Mild dysplasia or
mild dyskaryosis
CIN-1
LSIL
Low grade CIN
Moderate dysplasia
or moderate
dyskaryosis
CIN-2
HSIL
High grade CIN
Severe dysplasia or
severe dyskaryosis
CIN-3
HSIL
High grade CIN
Carcinoma in situ
CIN-3
HSIL
High grade CIN
Invasive carcinoma
Invasive
Invasive
Invasive
36
DR.Maninder Ahuja VP FOGSI
4/8/2015
Properties and charactristics of different screening methods
Screening test
Sensitivity
Cytology
Low to moderate
44-78%
HPV DNA
High(66-100%)
Specificity
high 91-96%
Requires health
based
infrastructure,laborat
ory , training,
subjective
Moderate (61-90%)
Lab based,
objective,repruducibl
e, expensive
Visual inspection
37
characteristics
Low technology, low
cost ,linkage to
immediate treatment
VIA
Moderate 67-79%
Low 49-86%
VILLI
Moderate high 7898%
Moderate 73-93%
DR.Maninder Ahuja VP FOGSI
Suitable for low
resource settings
4/8/2015
Poor-Moderate Sensitivity of Cytology
38
DR.Maninder Ahuja VP FOGSI
4/8/2015
Sensitivity of a single HPV test
39
DR.Maninder Ahuja VP FOGSI
4/8/2015
Cyto. Dx & Associated High Grade Lesions
Incidence
CIN 2/3
Invasive Ca
ASC-CU
2.5 to 5.0%
5-10%
<0.1%
LSIL
1.5 to 2.0%
15-30%
0.1-0.2%
HSIL
0.5 %
70%
1-2%
Glandular abnormalities: Colposcopy+ ECC is recommended
40
DR.Maninder Ahuja VP FOGSI
4/8/2015
Disadvantages of Cytology
Sensitivity of single smear is 51% & specificity is
98%.
Expensive, Requires infrastructure and training
2/3rd of false negatives are due to errors of
sampling.
40-50% cancers in cases screened within 5 years .
15-42% fail to obtain evaluation.
10-18% are never notified.
41
DR.Maninder Ahuja VP FOGSI
4/8/2015