Transfusion talk for GIM 2013 - University of Colorado Denver
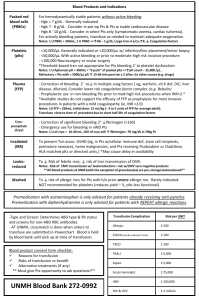
advertisement

• Anemia, Oxygen Delivery – Physiology – Clinical evidence for RBCs – Sepsis, CAD/ACS, Trauma • Coagulopathy – Physiology – Clinical evidence for FFP use – Liver disease • Thrombocytopenia – Evidence-based use of Platelets – Uremia Translate what you learn today to our trainees and change the transfusion culture in Colorado Help practitioners/educators: Develop a framework for performing risk/benefit analysis for each transfusion decision To understand the clinical and physiologic evidence behind those decisions To challenge dogmatic transfusion practices based on new evidence Risk Febrile transfusion reactions Allergic reaction Anaphylaxis HIV Hepatitis B Terrible T’s TRIM TRALI TACO Incidence <1 in 100 2-3 in 100 2 in 100,000 1 in 2,000,000 1 in 150,000 TRIM (transfusion-related immunomodulation) Reduce rejection (kidney transplants 1960s) Increased incidence of nosocomial bacterial infections Marik; CCM, 2008 Transfusion TRALI Other 12% Trauma 7% Pneumonia 35% Aspiration 11% NonPulmonary Sepsis 35% -6 hours 0 13% of all transfused MICU patients Mortality-8-9% Differentiating TACO and TRALI BNP Hypertension vs. Hypotension Leukopenia or fever (TRALI) Diurese to low pulmonary venous pressures Trial of diuresis Hypoperfusion TRALI Trial of diuresis Resolution TACO RBC (acquisition cost) ~$200 per unit RBC (total cost) ~$1400-$2400 per unit Higher if you factor in care for probable complications ▪ TRALI (8% incidence in ICU) ▪ Nosocomial infection (10% increase per unit) Transfusion TRALI Other 12% Trauma 7% Pneumonia 35% Aspiration 11% NonPulmonary Sepsis 35% -6 hours 0 Red Blood Cell Transfusion 1) Physiologic 2) Hard outcome 3) Symptom? Transfusion reactions TRALI TACO (hydrostatic edema) TRIM (nosocomial infection) Cost ($ and Human) 76YM w/ HTN, CAD (Hx MI) admitted to the ICU with pneumonia severe sepsis Quickly improved with IVF (5L), oxygen, antibiotics overnight- transferred to floor BP- 110/50 (140/90), HR 110, Temp-100.8 SPO2 90% on 4LNCO2 Lactate-4.8 2.8, Hgb 9.67.6, Creatinine 1.81.4 (0.8) BP- 110/50 (140/90) HR 110, Temp-100.8 1) Physiologic SPO2 90% on 4LNCO2 2) Hard outcome 3) Symptom? Lactate-4.8 2.8 Creatinine- 1.81.4 (0.8) Transfusion reactions TRALI TACO (hydrostatic edema) TRIM (post-transfusion infection) Cost ($ and Human) Hgb 9.27.6 Physiologic benefit RBCs SPO2 x Hgb x CO (SV x HR) Hgb=3.5 Heart rate (beats/min) = 116 - 4.0 x Hgb (g/dL) Zimmerman; Critical Care Med, 2004 1st case- Epi Q’s re: anemia and transfusion Need hospital transfusion numbers 2nd case: Sepsis: APACHE II<20, 52YM, increase O2 delivery?, Improve outcome benefit? When? Harm? Leukoreduction? 3rd case: Post-op knee 55YM: AF w/ RVR, known CAD, improve myocardial O2 delivery? rehab potential? ADLs? 4th case: NSTEMI (HCT 25), AF w/ RVR, No EKG changes, transitions to STEMI Age of blood? Everything else is extrapolation from these studies Do summary slide here of key points (with pictures) Incidence: X% at 3 days Mechanisms (non-bleeding) Loss (phlebotomy) ▪ Sepsis; X% total hgb drop Suppression (TNF, IL-1, IL-6) ▪ ↓ Epo + Epo receptor ▪ Induce apoptosis of erythroblasts ▪ Decreased availability of Iron Destruction-RES system Dilution Epidemiology of Transfusion in the Critically Ill Napolitano; Critical Care, 2004 PROPENSITY MATCHED 30 DAY MORTALITY Adj 30d Mort: 1.65, p< 0.001 ABC Study Outcomes (Europe) Difference in Mortality by Number of Units Transfused. Vincent, J. L. et al. JAMA 2002;288:1499-1507 Copyright restrictions may apply. ABC Study Outcomes Survival Analysis by Transfusion Status Among Propensity-Matched Patients. 28-day mortality 23% vs. 17%, p=0.05 Vincent, J. L. et al. JAMA 2002;288:1499-1507 Copyright restrictions may apply. Transfusion TRALI Other 12% Trauma 7% Pneumonia 35% Aspiration 11% NonPulmonary Sepsis 35% -6 hours 0 Multicenter RCT, Canada, n=838 Hgb 7 vs. 10 Who: non-bleeding, CAD (600 ex) Ischemic heart disease (n=257) Outcomes 30d Mortality 18% vs. 23%, p=.10 Hospital Mort 22% vs. 28%,p=.05 Subgroups APACHE II < 20 (9% vs 16%, p=.03) Age < 55 (5.7% vs. 13%, p=.02) Hebert; NEJM, 1999 Complications ▪ ARDS or pulmonary edema (8% vs. 14%, p<.01) ▪ MI (0.7% vs 2.9%), p=.02 Multicenter RCT, US/Canada, n=2016 Hgb 7 vs. 10 Who: age> 50, Hip repair Clinical evidence/RF Heart disease Hgb <10 w/in 3d surgery Outcomes 60d mort/10 ft: 35% vs. 35%, p=.90 MI/UA/Death: No difference Discharge Location Functional outcomes (Fatigue, ADL) Notes 2 units. vs. 0 units 1.3 g/dL difference nadir hgb Carson, NEJM, 2012 Complications ▪ No differences in 20+ transfusion outcomes DO2 = CO x (SPO2 x hgb) Oxygen kinetics? Will ↑RBCs ↑O2 utilization Assumptions: transfused RBCs ▪ Don’t alter the flow (CO) ▪ No alteration inO2 kinetics ↑DO2 ≠ ↑VO2 1) delivery dependent hypoxia 2) microvascular delivery 3) 0xygen kinetics maintained Transfused RBCs : Greedy Flow, O2 kinetics Fragile Autoregulation, plugging Sticky adhesionshunting microvesicles 16 pt- Septic Shock and hgb <10g/dl 1) Dobutamine 10mcg 800cc RBCs (3 units) 2) 800cc RBCs (3 units) Dobutamine 10mcg DO2 (jncreases in both scenarios) Dobutamine 48.5 (± 6.9) PRBCs 21.3 (± 4.3) VO2 increased only with Dobutamine 21.7 (Dobutamine) vs. 2.2 (PRBCs) Conclusion: In septic patients with delivery (DO2) dependent decreases in VO2, RBC transfusion does not improve VO2. Lorente; Critical Care Med, 1993 Zimmerman; Critical Care Med, 2004 The storage lesion (average US age=17 days) ↓deformability, ↑ fragility Loss of antioxidantsHgbMethemoglobin Lose 2,3 DPG (7-14 days), ATP, NO WBC may accelerate storage lesion ▪ ↑ IL-1, IL-8, TNF, bioactive lipids, HLA-ag Epidemiology (all RBCs>14d) ↑ PNA, infxn, MOF, LOS in TRAUMA ↑ Morbidity/Mortality in Cardiac Surgery ▪ 2 RCTs ongoing (10/14d vs. 21) Interventional Studies (MICU) Physiologic outcomes with inconsistent results ABLE (Age of Blood Evaluation) ICU Patients ▪ n=2510, 25 centers Canadian, double blind RCT ▪ Vent >48 hours, ICU, request for 1 RBC unit ▪ Fresh (<7d) vs. standard (15-20d) ▪ 90day mortality (power 25%20%) Epidemiology ▪ Association with TRALI, infection, mortality Universal leukoreduction- 2005 in US No outcome benefit before and after studies No benefit in recent RCTs (Trauma/Med/Surg) Mortality, Infection, TRALI Except CABG less post-op infection Should we switch back to non-leukoreduced blood? more economical CAD/ACS Myocardium oxygen extraction ratio- 55-70% CAD or ACS flow limited Do RBCs increase DO2 myocardial VO2? Transfused RBCs NO sink, ↓ ATP, reduce microvascular flow Hypercoaguable, ↑platelet aggregation ↓worsening oxygen kinetics 24,112 patients from 3 ACS (NSTEMI) trials 10% (2401) transfused Adjusted for 50+ co-morbidities and time from admission Grouped by nadir HCT; 20-25%, 25-30%, >30% Adj. probability of death at 30d w/transfusion Rao; JAMA, 2004 39, 922 pts, ACS (NSTEMI and STEMI) STEMI- Improved outcomes when transfused up to Hgb≥ 12 g/dL NSTEMI- Worse outcomes when transfused at any Hgb level!! Registry: ACS patients: Worse CV outcome and death with transfusion down to hgb < 9 g/dL (equivalent below 9 g/dL) Sabatine; Circulation, 2005 Singla; Am J Card, 2007 TRICC-(357 -CV disease), (257-IHD) Hgb-7 vs 10 g/dL No difference in 30 day mortality (0.3%) FOCUS- 2016 CAD or RF for CAD, Age>50 Hgb-7 vs 10 g/dL No difference in mortality or functional outcomes STEMI Up to Hct 30% if active ischemia? NSTEMI Up to Hct 20-25% if active ischemia?? CAD (no active ischemia) hgb 7mg/dL (FOCUS) Alternatives to increase supply and reduce demand Reverse or avoid inadequate tissue oxygenation due to inadequate delivery Transfusion reactions TRALI TACO (hydrostatic edema) TRIM (nosocomial infection) Cost ($ and Human) Risk Febrile transfusion reactions Allergic reaction Anaphylaxis HIV Hepatitis B Terrible T’s TRIM TRALI TACO Incidence <1 in 100 2-3 in 100 2 in 100,000 1 in 2,000,000 1 in 150,000 TRIM (transfusion-related immunomodulation) Reduce rejection (kidney transplants 1960s) Increased incidence of nosocomial bacterial infections Marik; CCM, 2008 Within 6 hours ALI Dx criteria 1) Acute 2) Bilateral infiltrates 3) Hypoxemia 4) Not hydrostatic edema (TACO) Associated most commonly with platelets and plasma Mortality 30-50% in ICU patients Antibody mediated (Anti-HLA I or II, Anti-neutrophil) Non immune mediated Common-5-8% MICU pts transfused (29% bleeding liver disease) Massive transfusion studies No analysis of FFP Recent ALI association studies have identified FFP as an independent risk factor (9 studies) Ruptured AAA repair(1) , MICU (3), trauma (2) mechanically ventilated (2), Sepsis (1) No association of RBCs and ALI when adjust for FFP FFP/Plts most common causative agents TRALI in critically ill MICU TRALI incidence: 5-8% transfused pts Mortality- 41-53% Benson, ICM, 2010 Vlaar, CCM, 2010 Gajic O, TRALI in the Critically ill, AJRCCM 2007 Benson, ICM, 2010 Silliman C, Blood 2003 Wallis JP, Transfusion 2003 13% of all transfused MICU patients Mortality-8-9% Differentiating TACO and TRALI BNP Hypertension vs. Hypotension Leukopenia or fever (TRALI) Diurese to low pulmonary venous pressures Trial of diuresis Hypoperfusion TRALI Trial of diuresis Resolution TACO RBC (acquisition cost) ~$200 per unit RBC (total cost) ~$1400-$2400 per unit Higher if factor in care for probable complications ▪ TRALI (8% incidence in ICU) ▪ Nosocomial infection (10% increase per unit) Reverse or Avoid inadequate tissue oxygenation due to inadequate delivery Transfusion reactions TRALI TACO (hydrostatic edema) Infection (TRIM) Cost ($ and Human) Special Populations: CAD/ACS Sepsis Trauma All blood products associated with morbidity and mortality in dose-dependent manner TRALI Infection MOF Ratio debate: FFP:PRBC:Plts Bleeding control? Coagulopathy? TRICC approach (hgb=7) safe and effective postresuscitation Most hospital have a protocol RBCs:FFP~2:1 General measures: Ionized Calcium > 0.9 mmol/L pH >7.10 Temperature > 34 degrees Plug hole in vessel!! Pressure on hole (allow time for clotting) Change pressure gradient in vessel ▪ Embolization, lower driving pressure (hypotensive resuscitation) 1.0 1.5 2.0 Reduce Bleeding Transfusion complications 3.0 1) Thoracentesis and elevated INR (Coumadin)? LP? Go over pre-procedure prophylaxis data 2) Liver disease paracentesis GI bleed (elevated INR) Dose (use of vit K), what if bleeding 3) Really (18) High INR on Coumadin Head bleed, Factor VIIa? 5) Uremia procedure- what to do? 6) PNA, malignancy- Plts 20k 1.5 3.0 Prevent Bleeding? Stop Bleeding? Transfusion complications Gajic; Critical Care Med, 2006 If Bleeding and Coagulopathy 2010 AABB guidelines: consider FFP for: Yes: ▪ Massive transfusion < 1:3 ratio (moderate/low grade) ▪ Coumadin induced ICH (very low grade) Neutral ▪ Surgery/Trauma (no massive transfusion) (very low) NO ▪ Coumadin high INR No ICH (very low) ▪ All non-bleeding situations (silent on liver disease) Central lines Arterial Lines Thoracentesis Liver disease Paracentesis Percutaneous/Transjugular liver biopsy Prior to banding for nonbleeding varices Dental extraction (use DDAVP) The INR=1.5 story Prothrombin time > 1.5 x upper limit normal: ▪ safe to perform surgery with normal hemostasis ISI developed to standardize tissue factor ISI in most labs was 1 1:1 relationship btw PT > 1.5 x ULM and INR=1.5 Now back calculation yield an INR-1.8-2.2 ▪ normal hemostasis Transfusing Platelets 44% of ICU patients thrombocytopenia Transfusion Triggers: No bleeding RF: <10k; bleeding RF???: <20k Large vessel Bleeding: 50k -60k Diffuse microvascular bleeding: 100k Pre-procedural prophylaxis: 50k; Surgical prophylaxis: 100k Measure plts 1 hour after to evaluate for consumption/destruction Main risk TRALI (highest of all blood products) Mechanism: Altered GP1B, ↓IIb/IIIa receptors (adhesion/aggregation) Dysfunctional vWF, Less functional factor VIII Plts↑ PGI2 levels, ↓plt TxA2, ADP Effects uremic toxins/anemia Treatment: (BUN does not correlate) Dialysis **Desmopressin (48h) , *Cryoprecipitate (1 h onset) EPO/Transfuse to HCT=30 Estrogen (0.6mg/kg IV QD x 5d) 134 trauma patients randomized to Novo VIIa after 6 units of blood in 4 hours ARDS 16% vs. 4%, p= .03 Boffard KD, J Trauma 2005