Learner Version Module 30 Created by Michael Reyes MD, and
advertisement

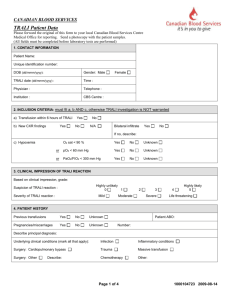
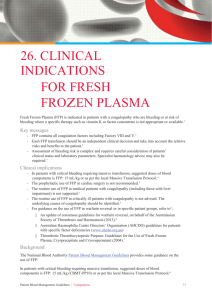
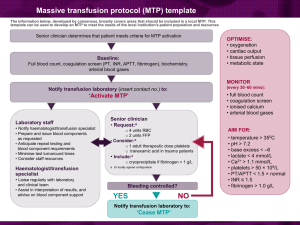
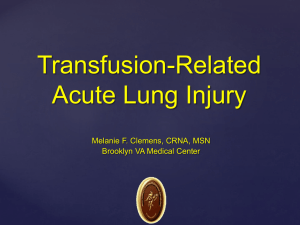
Learner Version Module 30 Created by Michael Reyes MD, and Sara Koenig MD 4/14 Objectives: See Facilitator Version References: See Facilitator Version Case A 68 year old male with a history of chronic lymphocytic leukemia, hypertension, and cirrhosis secondary to alcohol abuse presents to the ED following a brief episode of melena. His medications include fludarabine, lisinopril, metoprolol, and diazepam for occasional anxiety. On physical examination, his temperature is 37.3 degrees Celsius, blood pressure is 150/90 mm Hg, pulse is 90/minute, respiratory rate is 16/min, and O2sat is 97% on room air. There is no scleral icterus or jaundice, however trace bilateral lower extremity edema is present. There is no evidence of ascites. The patient’s spleen is mildly enlarged and non-tender. The patient weighs 100 kg. Labs: Wbc 16, Hgb 11, Hct 33, Plt 80, LFTs: AST: 320, ALT:90, TP 5.3 g/dL, TB 3.1, DB 0.8, Chem7 normal, INR 1.5, PT 15s, PTT 38s The patient is admitted to Blue Medicine and a GI consult is obtained to identify the source of the melena. GI says that they will not “scope” the patient unless the INR is less than 1.5. They recommend FFP to lower the INR prior to endoscopy. What are the common indications for FFP? What are some of the potential complications of transfusing FFP? Is FFP likely to be helpful in this patient whose melena has resolved? What is a therapeutic dose of FFP? Does this patient’s FFP need to be irradiated? Despite pleading with GI regarding the lack of an indication for the 2 units of FFP in this patient who is not currently bleeding with a mildly elevated INR, you give in to their request as they will not perform endoscopy without pre-procedure FFP. The patient receives 2 units of FFP. About half way through the second unit of FFP the patient’s nurse notices that he has developed a fever of 38.7 degrees Celsius. All other vital signs are normal, and the patient reports no clinical symptoms. The patient’s nurse calls the Blue Medicine Resident, reports the fever, and asks how to proceed. What is the very first thing you will tell the nurse? What further steps should be taken in this suspected transfusion reaction? What is your differential diagnosis at this point? While waiting for the suspected transfusion reaction testing to come back, the patient’s nurse calls you back and says that the patient has developed severe shortness of breath and is requiring supplemental oxygen to keep his O2 sats around 90. Based on the current symptoms, what is your differential diagnosis now? Which studies/lab tests will you order/what other information should be assessed? The results of the suspected transfusion reaction work-up and of the other studies are now available, and are as follows: The following studies were negative/no discrepancy: Bedside clerical check, BB clerical check, DAT, serum hemoglobin, ABO and Rh type. The patient’s vitals are as follows: Pre-transfusion: Pulse 84, Temp. 37.3, RR 12, BP 150/92, O2sat. 97% on RA At time of reaction: Pulse 110, Temp. 38.7, RR 28, BP 135/82, O2sat. 80% on RA The chest x-ray shows a bilateral “whiteout” consistent with pulmonary edema. The patient’s pre- and post-transfusion BNPs are similar and within the normal range and a stat ECG shows normal rhythm with sinus tachycardia. Following review of the patient’s symptoms, the suspected transfusion reaction results, vitals, and additional testing, a preliminary diagnosis of TRALI is made. Reaction TACO Signs and Symptoms Dyspnea, hypertension, pulmonary edema, JVD, peripheral edema, increased pulmonary capillary Studies/Labs BNP (pre- and posttransfusion), chest Xray Usual Cause Rapid/excessive infusion of blood products in at risk patients (CHF, MI, renal failure, etc.) Treatment Stop transfusion, diuresis, supportive care Prevention Avoid rapid or excessive infusion of blood products— especially in at risk patients, use low volume products if TRALI wedge pressure Dyspnea, hypoxemia, fever, hypotension, pulmonary edema, normal pulmonary capillary wedge pressure Chest X-ray, BNP (to r/o TACO), labs to assess for hemolysis (r/o hemolytic transfusion reaction) Donor HLA or antineutrophil antibodies Supportive care, intubation if severe symptoms necessary Deferral of high risk donors, reporting and deferral of TRALI associated donors ** All signs and symptoms may not be present for any given reaction A diagnosis of Transfusion related acute lung injury (TRALI) is made. The patient continues to deteriorate and requires emergent transfer to the MICU and intubation. The patient’s MICU course is uneventful and following resolution of his pulmonary edema he is eventually extubated. No further episodes of melena are reported during his inpatient stay and he is eventually discharged with an appointment to see GI as an outpatient. Describe the pathophysiology of TRALI Is this patient at increased risk of TRALI with future transfusions? Which blood products are most associated with TRALI? How is TRALI managed? How have blood banks sought to minimize the risk of TRALI? Associated Transfusion MKSAP questions for this module: Hematology Question 3 Question 7 Question 14 Question 50 Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111), or give to Dr. Patrick Rendon, UNM Hospital Division of Hospital Medicine 4 ACC. 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle) 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student