Dr-Kevin-Patterson
advertisement

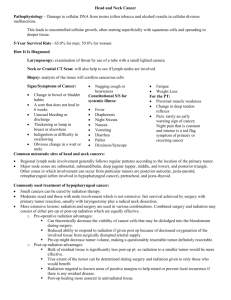
Dr Kevin Patterson TQEH EPIDEMIOLOGY SA CANCER REGISTRY 2003 119 new cases “cancer of the brain”(primary malignant tumours arising in the brain) 67 male, 52 female 9 in the 15-19 age group 24 in 20-44 age group Remainder (86) 45 + age group CONT. 50 (42%) in >65 yo age group Incidence increases with age particularly for high grade tumours TYPES OF TUMOUR RAH neurosurgical data 1977-98 80 % Astrocytoma 20% variety of other tumours including oligodendroglioma, ependymoma, medullo blastoma, other glial tumours not otherwise classified and primary CNS lymphoma CONT. Majority in RAH data (90%) were high grade tumours (GLIOBLASTOMA) In terms of burden of disease in adults high grade gliomas represent the largest single group Treatment Options Surgery cornerstone of initial management Purpose of surgery is diagnostic and therapeutic Increasing evidence that extent of resection (biopsy vs sub-total resection vs total resection) impacts on outcome Whats’s New in Surgery? Functional MRI (fMRI): This newer type of MRI looks for tiny blood flow changes in an active part of the brain. It can be used to determine what part of the brain handles a function such as speech, thought, sensation, or movement. Doctors can use this to determine which parts of the brain to avoid when planning surgery or radiation therapy. Awake Craniotomy In some cases, tumors infiltrate parts of the brain involved in movement or language. In such cases, functional intraoperative mapping can help identify the exact location of these functions in the brain, enabling the surgeon to avoid these areas and thereby minimize the risk of harm to the patient during surgery. This mapping process often requires that patients remain awake during surgery, especially in the case of speech mapping. FGS Fluorescence-guided surgery. For this approach, the patient drinks a special fluorescent dye a few hours before surgery. The dye is taken up mainly by the tumor, which then glows when the surgeon looks at it under special lighting from the operating microscope. This lets the surgeon better separate tumor from normal brain tissue. Radiotherapy Well established treatment for high and lower grade tumours post surgery May be primary treatment modality if surgery inappropriate Important to avoid radiation exposure to “normal” brain because of TOXICITY Standard RT delivered to tumour plus a margin RT delivery methods Three-dimensional conformal radiation therapy (3D-CRT) Intensity modulated radiation therapy (IMRT) Conformal proton beam radiation therapy RT delivery methods Stereotactic radiosurgery/stereotactic radiotherapy: This type of treatment delivers a large, precise radiation dose to the tumor area in a single session (radiosurgery) or in a few sessions (radiotherapy) RT delivery methods In one approach, radiation beams are focused at the tumor from hundreds of different angles for a short period of time. Each beam alone is weak, but they all converge at the tumor to give a higher dose of radiation. An example of such a machine is the Gamma Knife. RT delivery methods Another approach uses a movable linear accelerator (a machine that creates radiation) that is controlled by a computer. Instead of delivering many beams at once, this machine moves around the head to deliver radiation to the tumor from many different angles. Several machines with names such as X-Knife, CyberKnife, and Clinac are used in this way for stereotactic radiosurgery RT delivery methods Brachytherapy (internal radiotherapy): Unlike the external radiation approaches above, brachytherapy involves inserting radioactive material directly into or near the tumor. The radiation it gives off travels a very short distance, so it affects only the tumor. This technique is most often used along with external radiation. It provides a high dose of radiation at the tumor site, while the external radiation treats nearby areas with a lower dose. Chemotherapy Commonly used as an adjunct to surgery/RT (concurrent Temozolomide/RT in GBM) or salvage Problem with drug delivery is the BBB Progress has been slow with a number of negative trials reported in recent years Angiogenesis inhibitors Bevacizumab (Avastin) most well established Approved and funded in USA for treatment of relapsed GBM (not funded in Australia) First line trials in combination with standard CT/RT have not demonstrated a survival advantage Local Delivery Gliadel (carmustine) wafers Implanted at time of surgery and slowly release chemotherapy locally Randomised trial has demonstrated benefit over surgery/RT alone in GBM No data to compare with standard RT/Temozolomide Local delivery For a newer method called convection enhanced delivery, small tubes are placed into the tumor in the brain through a small hole in the skull during surgery. The tubing extends through the scalp and is connected to an infusion pump, through which chemo drugs can be given. This may be done for hours or days and may be repeated more than once, depending on the drug used. This is still an investigational method, and studies are continuing. New approaches “Targeted” therapies, recognise a unique genetic defect in the tumour that drives growth or prevents cell death eg activating EGFR mutations Currently small molecule TKI’s and monoclonal AB’s most well developed Immunotherapy Need to “persuade” the immune system to recognise tumour as foreign and mount an immune response against the tumour Personalised vaccines use tumour from individual patients to prime immune cells which are re-injected (dendritic cells) Immunotherapy Protein vaccines which provoke an immune response against a particular molecule on the tumour eg EGFR VIII This is a mutation of the EGFR receptor present on 1/3 of GBM Phase 3 trial currently ongoing Other approaches Hypoxic cell sensitisers Therapeutic viruses Trials in Australia http://www.cancertrialsaustralia.com/Clini cal-Trials-Register.aspx Calvary North Adelaide, relapsed GBM, carboplatin or lomustine in combination with Buparlisib (PI3K inhibitor) Support and Community Services Adelaide Brain Cancer Support group Cancer Council…………. Huge unmet need for brain cancer coordinator THANKYOU