Head and Neck Cancer
advertisement
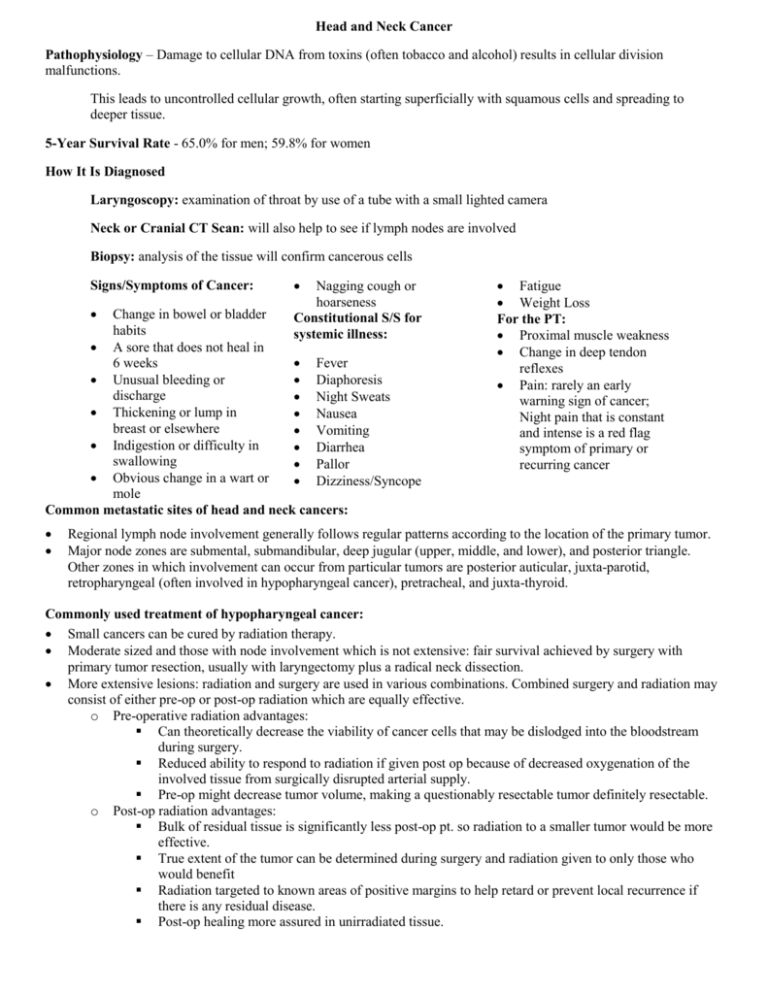
Head and Neck Cancer Pathophysiology – Damage to cellular DNA from toxins (often tobacco and alcohol) results in cellular division malfunctions. This leads to uncontrolled cellular growth, often starting superficially with squamous cells and spreading to deeper tissue. 5-Year Survival Rate - 65.0% for men; 59.8% for women How It Is Diagnosed Laryngoscopy: examination of throat by use of a tube with a small lighted camera Neck or Cranial CT Scan: will also help to see if lymph nodes are involved Biopsy: analysis of the tissue will confirm cancerous cells Signs/Symptoms of Cancer: Nagging cough or hoarseness Constitutional S/S for systemic illness: Change in bowel or bladder habits A sore that does not heal in Fever 6 weeks Unusual bleeding or Diaphoresis discharge Night Sweats Thickening or lump in Nausea breast or elsewhere Vomiting Indigestion or difficulty in Diarrhea swallowing Pallor Obvious change in a wart or Dizziness/Syncope mole Common metastatic sites of head and neck cancers: Fatigue Weight Loss For the PT: Proximal muscle weakness Change in deep tendon reflexes Pain: rarely an early warning sign of cancer; Night pain that is constant and intense is a red flag symptom of primary or recurring cancer Regional lymph node involvement generally follows regular patterns according to the location of the primary tumor. Major node zones are submental, submandibular, deep jugular (upper, middle, and lower), and posterior triangle. Other zones in which involvement can occur from particular tumors are posterior auticular, juxta-parotid, retropharyngeal (often involved in hypopharyngeal cancer), pretracheal, and juxta-thyroid. Commonly used treatment of hypopharyngeal cancer: Small cancers can be cured by radiation therapy. Moderate sized and those with node involvement which is not extensive: fair survival achieved by surgery with primary tumor resection, usually with laryngectomy plus a radical neck dissection. More extensive lesions: radiation and surgery are used in various combinations. Combined surgery and radiation may consist of either pre-op or post-op radiation which are equally effective. o Pre-operative radiation advantages: Can theoretically decrease the viability of cancer cells that may be dislodged into the bloodstream during surgery. Reduced ability to respond to radiation if given post op because of decreased oxygenation of the involved tissue from surgically disrupted arterial supply. Pre-op might decrease tumor volume, making a questionably resectable tumor definitely resectable. o Post-op radiation advantages: Bulk of residual tissue is significantly less post-op pt. so radiation to a smaller tumor would be more effective. True extent of the tumor can be determined during surgery and radiation given to only those who would benefit Radiation targeted to known areas of positive margins to help retard or prevent local recurrence if there is any residual disease. Post-op healing more assured in unirradiated tissue. Chemotherapy: single and combination; no evidence that chemotherapy increases prognosis; mainly used for unresectable, recurrent, or metastatic cancer in which reradiation cannot be delivered (median duration of survival in this case is 6 months). No standard single agent for therapy for advanced head and neck cancer Radical Neck Dissection: Unilateral cervical lymphadenectomy in which a block of tissue is removed from the level of the clavicle below up to the mandible above, from the trapezius muscle posteriorly to near the midline anteriorly. SCM and omohyoid muscles and jugular vein are included. In modified neck dissections internal jugular vein, spinal accessory nerve, SCM, or all 3 may be preserved. Carotid blowout Can be a complication in patients with head and neck malignancy Radiation o Decreases blood flow to carotid artery o Less blood flow mean it’s easier for the artery to rupture Precautions in Physical therapy for a patient with a risk of carotid blowout o Be gentle with cervical stretching and ROM in the acute phase o Be gentle with any scar massage in the acute phase o Be cautious when doing neck musculature strengthening not to overstrain But it can happen…and the patient can die from hypovolemic shock in minutes Symptoms preceding a carotid blowout o salivary fistula - An opening between a salivary duct or gland and the skin surface or the oral cavity. o Local infection o ‘herald bleed’ – A brisk gastrointestinal bleed that stops spontaneously, then recurs hours later If it happens o Apply pressure to stop bleeding o Call for nursing or medical support o Send out crash call or call 911 The risk of carotid artery rupture has been virtually eliminated because of several factors: o radiation therapy is usually administered postoperatively (within 4-6 wk of surgery), which allows for healing prior to the start of effects. o muscle flaps that can cover the carotid artery provide it with a healthy source of uninvolved, unirradiated (not having been exposed to radiation) tissue Carotid rupture today, when it occurs, usually is preceded by a history of radiation therapy, tumor erosion into the carotid artery, and the development of a fistula to the aerodigestive tract Psychosocial Aspects: • • • • Patients with cancer may experience depression upon being diagnosed, this depression often worsens as they begin aggressive and painful treatments such as chemotherapy. Because they are so ill, many cancer patients are no longer able to work and enjoy leisure activities they did prior to illness. This causes them to be isolated and feel very alone at times. As PTs, we need to motivate cancer patients by emphasizing strengths, giving positive feedback, and empowering patients with activities that they will succeed in. If you suspect that your patient may be depressed, refer them to a psychologist. References submitted, but not included, due to space limitations