The ECMO Effect
advertisement

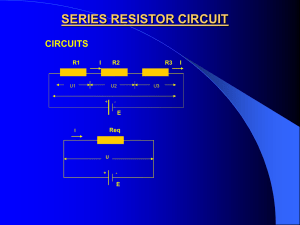
Medications in the PICU: The ECMO Effect Lizbeth Hansen, PharmD, BCPS Angie Skoglund, PharmD, BCPS Clinical Pediatric Pharmacist University of Minnesota Amplatz Children’s Hospital Objectives Discuss pharmacologic principles of analgesia, sedation and paralysis Review the current data that addresses the effect of ECMO (extracorporeal membranous oxygenation) on commonly used medications Analgesia, Sedation & Paralysis Opioid Analgesics Mechanism of Action Bind to opiate receptors (mu, gamma, kappa) Act on the descending inhibitory pathway in the CNS to produce analgesia As dose increases, so do side effects CNS depression Respiratory depression Nausea/Vomiting Constipation Urinary retention Opioid Analgesics Morphine Hydromorphone Fentanyl Initial dose (IV) 0.05-0.1 mg/kg 0.007-0.015 mg/kg 1-2 mcg/kg Continuous Infusion 0.03 mg/kg/hr 0.005 mg/kg/hr 1 mcg/kg/hr 2-4 minutes 2-4 minutes 1-2 minutes 2-4 hours 3-6 hours 30-60 minutes 10 mg 1.5 mg 0.1 mg Yes No No Onset of action Duration of action Equianalgesic dose Active Metabolite Clinical Pearls Morphine – histamine release responsible for hypotensive effects Fentanyl – too rapid administration of high doses can cause “rigid chest” phenomenon Sedatives Benzodiazepines Bind to the GABAA receptor to produce both anxiolytic and hypnotic effects Barbiturates Bind to a separate site on the GABA receptor to produce CNS depression (sedation) Sedatives Initial Dose (IV) Continuous Infusion Onset of Action Midazolam Lorazepam Propofol 0.05-0.1 mg/kg 0.05-0.1 mg/kg 1 mg/kg 0.05 -0.1 mg/kg/hr 0.025-0.05 mg/kg/hr 25-50 mcg/kg/min 2-4 minutes 15-30 minutes 30 seconds Duration of Action 1-2 hours 4-6 hours 3-10 minutes Active Metabolite Yes No No Phenobarbital Pentobarbital Initial Dose (IV) 1-3 mg/kg 1-3 mg/kg Onset of Action 5 minutes 1 minute Duration of Action 4-10 hours 15 minutes Dexmedetomidine MOA: highly selective alpha2 agonist Activation of alpha2 receptors in brain stem Sedation Activation of alpha2 receptors in spinal cord Analgesia Loading dose: 1 mcg/kg over 10 minutes then 0.2-0.7 mcg/kg/hr Adverse Effects Hypotension (25-50%), bradycardia (5-15%) Paralytics Depolarizing Neuromuscular Blockers Succinylcholine 1-1.5 mg/kg IV/IO RSI Onset: 2-3 minutes, Duration: 10-30 minutes Adverse effects: hyperkalemia, incr ICP, malignant hyperthermia Non-Depolarizing NMBs Initial Dose (IV) Continuous Infusion Onset of Action Duration of Action Elimination Vecuronium Cisatracurium Rocuronium 0.1 mg/kg 0.1 mg/kg 0.6-1 mg/kg 1-1.5 mcg/kg/min (0.05 -0.1 mg/kg/hr) 1-4 mcg/kg/min 10-12 mcg/kg/min 1-3 minutes 2-3 minutes 30-60 seconds 30-40 minutes 35-45 minutes 20-40 minutes Biliary (50%) Urine (25%) Hofmann elimination Biliary (70%) Urine (30%) ECMO Extracorporeal Membrane Oxygenation Prolonged form of cardio-pulmonary bypass (on average 3-10 days) Used to support patients with lifethreatening respiratory or cardiac failure Provides a decrease in workload and adequate oxygen to the patient while allowing time for the lungs and/or heart to “rest” or heal The ECMO Circuit The ECMO Circuit Components: Venous cannula (thru RIJ into RA), venous reservoir (bladder), roller pump, membrane oxygenator, heat exchanger, arterial cannula (thru RCA into AA) VA vs VV ECMO: Venoarterial ECMO bypasses lungs Venovenous ECMO does not provide cardiac support Indications Neonates Primary pulmonary hypertension, meconium aspiration, respiratory distress syndrome, group B streptococcal sepsis, congenital diaphragmatic hernia Infants & Children Low CO following repair of CHD Unable to wean off cardiac bypass in OR Bridge to cardiac surgery or transplant Complications Clots in circuit (19%) Oxygenator failure Seizures, intracranial bleeding Hemolysis & coagulopathy (SIRS) Arrhythmias Oliguria (within 24-48h) Metabolic acidosis Weaning Attempted daily by assessing systemic arterial and venous saturations when decreasing flow thru the bypass circuit When the required level of bypass flow is approx 10% of cardiac output, a trial period of ECMO should be done If patient able to maintain adequate gas exchange & acceptable hemodynamic parameters, decannulation can occur Medications Used in ECMO Inotropes and vasopressors for additional cardiac support Heparin to prevent clotting of ECMO circuit Antibiotics for prophylaxis and treatment of infection (vancomycin & 3rd gen ceph) Electrolyte supplementation Sedatives & analgesics for comfort Pharmaco-kinetic & -dynamic changes during ECMO Increased circulating blood volume Blood volumes needed to prime the circuit (300-400 mL) are more than double of the infant’s own blood volume (200-250 mL) Drug binding interactions with circuit Drug adsorption and sequestration onto plastic cannulae and/or silicone oxygenator Altered renal, hepatic & cerebral blood flow Non-pulsatile blood flow Previous injury to organs pre-ECMO Drug Administration into the ECMO circuit Dagan, et al (1993) showed decreases in serum concentrations while circulating through the ECMO circuit % change New circuit Used circuit (5 days) Morphine Phenytoin Vancomycin Gentamicin Phenobarb 36% 43% 36% 10% 17% 16% -- 11% 0% 6% The amount of drug lost to the circuit appears to be related to how new the circuit is Drug Administration into the ECMO circuit, cont’d Mulla et al (2000) showed significant decreases in serum concentrations due to uptake by the PVC tubing of ECMO circuit % Decrease Midazolam Lorazepam Diazepam Propofol No albumin 68% 40% 88% 98% Albumin 76% 52% 96% 99% When albumin was used to prime the circuit, they found an additional 10% increase in uptake of the sedatives Drug Administration into the ECMO circuit, cont’d Green, et al (1990) showed the clearance rate of heparin doubled while on ECMO compared to when decannulated 3.8 mL/kg/min vs 1.6 mL/kg/min Nearly 50% of the heparin dose lost in the circuit was Analgesics Fentanyl Up to 70% of the dose has been sequestered by the silicone membrane oxygenator Saturation kinetics – once the binding sites are saturated, less drug is needed to maintain sedation Morphine Dagan et al (1994) showed a decrease in clearance of morphine while on ECMO 34 mL/kg/min vs 63 mL/kg/min Authors postulated this may be an effect of decreased hepatic blood flow Phenobarbital In vitro studies have shown up to a 17% loss of a dose in a new circuit Increase in the Vd to 1.2 L/kg also leads to decreased concentrations in the blood Very important for serum drug monitoring to ensure patient is within therapeutic goal to prevent seizure activity Antibiotics Vancomycin Hoie (1990) & Amaker (1996) both showed an increase in Vd (0.68-1.1 L/kg) along with increase in half-life (7.7-16.9 hrs) Dose: 15-20 mg/kg IV q24h Gentamicin Cohen (1990) & Batt-Mehta (1992) both showed an increase in Vd (0.51-0.67 L/kg) along with increase in half-life (5.7-10 hrs) Dose: 2.5-3.5 mg/kg IV q18-24h Other drugs Due to lack of studies, it is unknown what pharmacokinetic changes occur during administration of other medications used to support the patient on ECMO Questions?