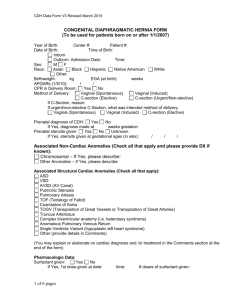
CDH Management Protocol
advertisement

CDH Management Protocol Antepartum (Fetal Center) • Level III ultrasound • LHR - Routinely calculated –if survival estimate less than ? % refer to PLUG center? • O/E LHR - Routinely calculated up to 32 weeks • Both LHR results will be listed on the bottom of the front StarPanel page • Cardiac echo - Routine • Liver position – Determined and reported • Multidisciplinary consults – MFM, NICU, Ped Surg, Genetics, etc Antepartum (Fetal Center) • • • • • Fetal MRI – Not standard (QLI) Follow-up – Monthly – BPP 2/wk at 34 wks Timing of delivery – Induction at 39 wks Antenatal steroids – For labor EGA < 34 wks Calculate LHR or O/E LHR: http://www.perinatology.com/calculators/ LHR.htm Delivery Room • Airway Management – No bag valve mask or CPAP. Immediate ETT for respiratory distress or BBO2 if stable • GI decompression – Replogle tube following airway • Ventilatory Pressures - 20-25/5-6 • FiO2 (initial) – 100% • Transport Vent - 20-25/5-6 x 40 It=0.35, FiO2=1 • SaO2 target - preductal increase no faster than NRP guidelines, wean FiO2 when preductal SaO2 up to >85% • iNO – if baby requires FiO2 of 100% NICU Stablilization • SaO2 (preductal) - >70% x 1 hour, >85% by 2 hours, goal 90-95% • Studies - Routine ECHO, HUS, cultures, PT/PTT, CBC, CRP, state screen, cortisol, karyotype & microarray? • Access – attempt single lumen UAC before peripheral a-line or UAC cut down (consult surgeon) – Single attempt UVC, if unsuccessful convert to emergent position, discuss PICC vs. Cook vs. other with team based on stability • Sedation - fentanyl 1mcg/kg/hr – additional dose for cardiac echo – add Versed as needed • Analgesia - fentanyl 1mcg/kg/hr • Paralysis - avoid Initial Ventilation Strategy • • • • • IMV - Initial settings PCV 22/5 x 40 It=.035 – Max RATE = 60 – Max PIP = 26 Oxygenation – Preductal sat > 70%x 1 hour, by 2 hours >85% with adequate delivery based on lactate, goal 90-95% – Post ductal PaO2 >40 (consider >35 with adequate preductal SaO2 and lactate) Ventilation – Goal = pCO2 50-65 pH - Goal = 7.2 – 7.35 Perfusion – O2 delivery with lactate < 3 mmol/L; transiently (2 hours) tolerable lactate >3, but <5 Weaning – wean PIP first with adequate tidal volume, then rate to SIMV when on low rate, volume based on PFT TV on prior setting, target 4-5 cc/kg – FiO2 to keep SaO2 90-95% – Wean PEEP slowly (decrease by 0.5 q4h) if FiO2<0.60 with 8 rib expansion High Frequency Ventilation • • • Criteria to Convert from CV to HFV – PaCO2 > 65 with acidosis on PIP 26 and rate 60 – Pre-SaO2<70% or post-ductal PaO2<40 when IMV has failed to achieve adequate (8-9 ribs) contralateral recruitment HFV initial settings – HFOV MAP=IMV MAP + 2 – Increase MAP to achieve 8-9 rib expansion contralateral to CDH – Delta P = PIP, “adequate bounce” – Starting frequency 10 Hz Weaning – Wean MAP slowly (decrease by 0.5 q4h) if FiO2<0.60 with 8 rib expansion (or 10 rib expansion?) – Wean frequency first to 10, then delta P to PaCO2 50-65 – FiO2 to keep SaO2 90-95% CDH Patient Management • • Systemic Hypotension - Criteria for treatment - Abnormal MAP for age – NS bolus, pRBC’s if Hct<40, FFP for abnormal initial coagulation studies – combined up to 40ml/kg in first 2 hours – Dopamine and Dobutamine - begin at 5/5 and increase as needed Pulmonary Hypertension - Criteria for treatment – Pre ductal SaO2<70% or post-ductal PaO2<40 AND echocardiographic evidence of PH – iNO • iNO at 20ppm, wean when FiO2<0.6 and adequate oxygenation – Prostacyclin • Reserved for rescue post-ECMO or where ECMO contraindicated • Consider inhaled for sustained hypoxemia on iNO if adequate ventilation and adequate contralateral lung recruitment can be achieved on conventional ventilator. Note: potential for platelet/bleeding effect – Catecholamines • to correct systemic hypotension into normal range after volume expansion and oxygen carrying capacity optimized – Milrinone • RV dysfunction/dilation and additional afterload reduction after iNO – Prostaglandin • Prostaglandin for RV overload with restrictive PDA CDH Patient Management • Fluid Management - Initial 90 ml/kg with early protein - Avoid fluid overload - Furosemide for fluid overload when hemodynamically stable • Laboratory Management - Hematocrit > 40% - Heparin assay (anti Xa) q6h, ATIII level QD (on ECMO) - Platelet count > 100,000 perioperatively (on ECMO) - TEG with clinical bleeding (on ECMO) Antibiotics - No specific indication for antibiotics with CDH alone - Evaluate maternal risk factors, initial sepsis screen - Start prior to cannulation Sedation - As clinically indicated - Paralysis should be avoided if possible, use with caution • • Criteria for ECMO • • • • • • • • SaO2<85% on HFOV and iNO HFOV MAP>17 OI>40 consistent (3 post-ductal BG over 2 hours) Inadequate oxygen delivery, pH<7.20, lactate>5 despite adequate volume expansion and pulmonary recruitment Respiratory acidosis despite optimized HFOV pH<7.20, PaCO2>70 Hypotension resistant to fluid and inotropic support with UOP<0.5ml/kg/hr Impending ventricular failure on ECHO with evidence of inadequate oxygen delivery Preductal sat <70 for 1 hour • Attending to Attending Notification ECMO Contraindications • IVH Grade 2 or greater • Lethal chromosomal anomalies/syndromes • Complex congenital heart disease (single ventricle physiology) • EGA < 35 wks CDH ECMO • • • • Echocardiographic Surveillance: – Cardiology to have Attending ECHO read upon arrival in NICU – Serial exams with at least one additional ECHO at 48h on ECMO ECMO Cannulation – Routine use of VA ECMO in CDH – Place 8 Fr arterial cannula – 12 Fr venous cannula or smaller Duration of ECMO Run – Duration of ECMO based upon a multidisciplinary review of the course and projected outcome / assessment of futility – Periodic trial of lower flows/trial off with echo assessment of PH Decannulation – Consider when trial off-EMCO suggests native gas exchange and CV function is sufficient • Ionotropic and ventilatory support should be below ECMO cannulation settings – Consider targeting higher PaCO2 range for final 3-7 days of ECMO run – Routine carotid artery repair unless contraindicated / unfeasible – Routine Broviac placement CDH Repair (no ECMO) FiO2<0.5 Normal BP for EGA Lactate <3 Pre-operative ECHO required demonstrating improvement in pulmonary hypertension and good right ventricular function • UOP > 2ml/kg/hr • Chest Tube – Consider no use of routine chest tube when repaired off ECMO • Location of Repair OFF ECMO: - In NICU with Pediatric Anesthesiology • • • • CDH Repair (ECMO) • Timing of repair will be based upon an ECHO after 48h on ECMO (maintain inflation until ECHO) – If there IS improvement in the pulmonary HTN (less than systemic) – delay repair (with a close eye on volume status), consider repair off ECMO – If there is NO improvement in the pulmonary HTN after 48h ECMO support – move towards early repair in 24-48h – If successfully weaned off ECMO – timing of surgery same as non ECMO babies (echo driven decisions) • Peri-Operative Anticoagulation Management – Hold heparin infusion 2 hours pre-op, during the case and 2 hours post-op – Restart heparin drip at pre-op rate, no bolus • Chest tube – Routine placement of chest tube (15f Blake drain) for repair done on ECMO • Temporary/Staged Abdominal Closure Outcomes • Routine analysis of institutional CDH registry data and morbidity assessment every 10 cases or 6 months (whichever occurs first) with departmental presentations