Aim
To show an in-depth understanding of the
genito-urinary disorders in children and the
process of care in the nursing management
By the end of this session, the student
should be able to:
Understand the anatomy and physiology of the renal
system and structure and function
Identify the differences between adult and children GU
system
Describe the most common diagnostic investigations and
procedures for GU disorders
Understand the general assessment of children with
genitourinary disorders
Understand the common genitourinary disorders in
children
Plan the nursing management for children with GU
disorders
Begins during 1st week of gestation
Completed by end of 1st year after birth
Excretion less than adult
By the age of 6 to 12 months, filtration and
absorption is nearly like adults
For healthy infant, the kidneys operate at a
functional level appropriate for the size of the
body.
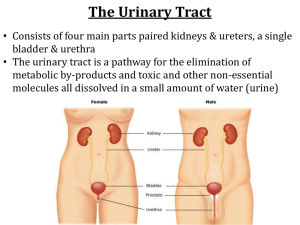
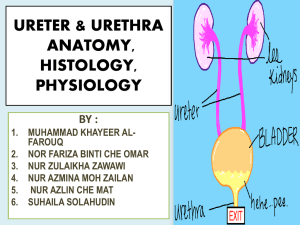
Nephron
Glomeruli – filter water and solutes from blood
Tubules – reabsorb needed substances (water,
protein, electrolytes, glucose, amino acids) from
filtrate and allow unneeded substances to leave
the body in urine
Urine formed in the nephron, passes into renal
pelvis, through ureter into bladder and out of body
through urethra
Urine formed in the nephron,
passes into renal pelvis, through
ureter into bladder and out of
body through urethra
Glomeruli :
filter water and solutes from
blood
Tubules :
reabsorb needed
substances (water,
protein, electrolytes,
glucose, amino acids)
from filtrate and allow
unneeded substances to
leave the body in urine
Maintaining body fluid volume and
composition
Secretes hormones: Renin
– helps with the regulation of blood
pressure
Erythropoietin – stimulates red blood cell
production by the bone marrow
Metabolised Vitamin D – responsible for
calcium metabolism
Urinalysis
CT Scan- an x-ray procedure that combines many
x-ray images with the aid of a computer to
generate cross-sectional views and, if needed,
three-dimensional images of the internal organs
and structures of the body.
gross indicator of renal function
(BUN) test measures the amount of nitrogen in blood that comes from the waste
product urea.
Urea is made when protein is broken down in body.
Blood urea nitrogen (BUN) and creatinine tests can be used together to find the BUN-tocreatinine ratio (BUN:creatinine). body in the urine.
A blood urea nitrogen (BUN) test is done to determine :
kidneys are working normally.
kidney disease is getting worse.
See if treatment of kidney disease is working.
See if severe dehydration is present. Dehydration generally causes BUN levels to rise more
than creatinine levels. This causes a high BUN-to-creatinine ratio. Kidney disease or
blockage of the flow of urine from kidney causes both BUN and creatinine levels to go up.
KUB (Kidney, Ureter, Bladder) x-ray
Renal Biopsy
Renal Ultrasound
An injection of x-ray contrast media via a needle or cannula into
the vein, typically in the arm. The contrast is excreted or
removed from the bloodstream via the kidneys, and the
contrast media becomes visible on x-rays almost immediately
after injection
a urologic procedure where the physician
injects contrast into the ureter in order to
visualize the ureter and kidney.
Micturating Cystourethrography (MCUG) – serial
x-ray of the bladder and urethra after IV
infusion of iodine-bound contrast medium ( to
detect blockage)
Urinary tract infection (UTI)
Nephrotic syndrome
Acute Post-Streptococcal
Glomerulonephritis (APSGN)
Vesicoureteral reflux
Hypospadias
Definition
UTI is the presence of bacteria in the urine
Infection usually occur at the upper urinary
tract or at the lower urinary tract
Incidence
Common age of onset for UTI is 2-6 years
Girl>Boy - Female has shorter urethra
Uncircumcised male prone to develop UTI
Causative organisms – E. Coli
Route of entry -bacteria ascending from the
area outside of the urethra.
Vesico-ureteral reflux
Infections – URTI, GE
Poor perineal hygiene - fecal organisms are
the most common infecting organisms due
to the proximity of the rectum to the
urethra.
Short female urethra
Urethritis – infection of the urethra
Cystitis – an infection in the bladder
that has moved up from the urethra
Pyelonephritis – a urinary infection
of the kidney as a result of an
infection in the urinary tract
Unexplained fever
(febrile fits)
Abdominal
pain
Poor
growth
Foul-smelling
urine
Irritability
Poor feeding
Vomiting
Weight loss
(failure to weight gain)
Urinary
frequency/urgency
Dysuria
Foul-smelling urine
Cloudy urine
Incontinence during
day and/or night
Increased irritability
Nausea and vomiting
Low abdominal or
flank pain
Fever and chills
Fatigue
Small amount of urine
while micturating
despite feeling of
urgency
Central pyrexia but peripherally cold
Poor colour
Pale, grey mottled skin
Quiet and lethargic child
Poor tone
Tachycardic and hypertensive
Obtaining a urine specimen:- Urine bag
- Clean catch urine
- Mid-stream urine
- Catheterisation
- Supra-pubic aspiration-draining the
bladder by inserting a sterile needle through
the skin above the pubic arch and into the
bladder.
Ultrasound
Plain x-ray
Micturating Cystourethrogram (MCUG)
Obtain urine specimen before antibiotics
started, sent for ME/CS
Blood tests
Strict I/O chart
Monitor vital signs esp. body temperature
Administer antibiotics as prescribed (5 days
course)
Administer anti-pyretic drugs to reduce
fever and pain
Advised to take plenty of fluids to prevent
dehydration and to flush the urinary tract
If the child is unable (vomiting) or refuse to
take fluids, administer IV fluids as
prescribed
Fever due to increased body temperature
related to urinary tract infection.
2. Alteration in urination (frequency, pain,
burning, dribbling and enuresis) related to
infection.
3. Pain related to inflammatory changes in
the urinary tract.
4. Lack of knowledge about UTI and health
prevention
1.
Goal: to reduce fever and maintain normal body temperature
Nursing interventions
Rationales
• monitor body temperature every 4º
• encourage plenty of fluid intake
• administer anti-pyrexial
medications as prescribed
• maintain bed rest
• wear thin loose clothing
• baseline obs.
• to maintain hydration
• to maintain an
optimum body temp.
• to reduce the body
heat
• give tepid-sponging with luke-warm • to reduce body heat
water
Problem 2: Alteration in urination (frequency, pain,
burning, dribbling and enuresis) related to infection
Goal: to ensure that the child is comfortable during urination
Nursing interventions
Rationales
• assess the urinary frequency, pain or • as baseline obs.
burning sensation during micturation
• assess the colour & odour of urine
• as baseline obs.
• strict I/O chart
• to observe urinary
frequency
• administer antibiotics as prescribed • to prevent spread
of infection
• to prevent
• observe for signs & symptoms of
complications
serious infection
Ensure the child to pass urine regularly
(every 2-3 hours) and take the time to
completely empty the bladder
Avoid holding urine for prolonged period of
time
Perineal hygiene - wipe from front to back
Avoid tight fitting clothing or diapers; wear
cotton panties
Avoid constipation
Encourage fluid intake
Avoid bubble baths
You are required to do the nursing care plan for
problem no. 3 & 4, including nursing
interventions and rationales
Alteration of glomerular
membrane permeability with
massive proteinuria,
hypoalbuminaemia,
hyperlipidaemia and oedema
It occurs when the filters in the kidney leak an
excessive amount of protein. The level of
protein in the blood ↓ and this allows fluid to
leak across the blood vessels into the tissues –
causing oedema
Nephrotic syndrome are caused by changes in
the immune system
For unknown reason, the glomerular
membrane, usually impermeable to large
proteins becomes permeable.
Protein, especially albumin, leaks through the
membrane and is lost in the urine.
Plasma proteins decrease as proteinuria
increase.
The colloidal osmotic pressure which holds water in
the vascular compartments is reduced owing to
decrease amount of serum albumin. This allows
fluid to flow from the capillaries into the
extracellular space, producing oedema.
Accumulation of fluid in the interstitial spaces and
peritoneal cavity is also increased by an
overproduction of aldosterone, which causes
retention of sodium.
There is increased susceptibility to infection due to
decreased gamma-globulin.
Causing generalised oedema
1 : 50 000 children
Males > females
Common age of onset is between 2 to 6 years,
but can occur at any age
Oedema
↓ urine output
- initially noted in the
periorbital area
- ascites
- intense scrotal
oedema
- striae may appear
due
to skin overstretching
- pitting oedema
↑ weight
Proteinuria (foamy urine
indicates proteinuria)
Fatigue
Irritable and depression
Severe recurrent
infections
Anorexia
Wasting of skeletal
muscles
Urinalysis
- protein 3+ - 4+ on dipstick
- haematuria may be absent or microscopic
Blood test
- total serum protein – low
- serum albumin – low
- cholesterol and lipoproteins – high
Renal function test – often normal
Blood pressure – often normal but 25%
hypertension
Renal biopsy
1.
2.
3.
4.
Generalised oedema due to fluid volume
excess related to glomerular dysfunction
Impaired skin integrity related to oedema
Altered urinary pattern related to glomerular
dysfunction
Increased susceptibility to infection related to
disease process and steroid therapy
5.
6.
7.
8.
Altered body image (round face) due to sideeffects of medication
Inadequate nutritional intake related to large
loss of protein from the urine
Knowledge deficit of the disease process and
treatment
Anxiety and depression due to the up and
down of the course of disease
Goal : to relieve oedema
Nursing interventions
Administer steroids – prednisolone 2-4mg/kg
to control oedema
Observe for side-effects of steroids – Cushing’s
syndrome (moon face, abdominal distension,
striae, ↑ appetite, ↑ weight, aggravation of
adolescent acne)
Administer diuretic – frusemide. Diuretics
can cause loss of electrolytes esp.
potassium, encourage ↑ potassium food e.g.
citrus fruits, date, apricot, banana
Keep the child CRIB during periods of severe
oedema
Strict I/O chart – restrict intake of fluid –
offer small amount of measured fluid during
severe oedema, for infant measure the
diaper’s wt.
Measure daily weight and abdominal girth –
to check any weight gain due to water
retention
Goal : to protect the child from skin
breakdown
Nursing intervention
Position the child comfortably in bed so that
oedematous skin is well-support with a
pillow
Elevate the child’s head to reduce periorbital oedema
Provide good skin care – give bath and
maintain hygiene esp. genitals and moist
area
Change bedding daily and free from creases
For problems 3 – 9, you are required to look for
the nursing interventions yourself.
Admission to ward
Explain to parents nature of illness
Blood for FBC/DC, U +E, Creat., Serum lipid,
C&S, LFT, serum albumin
For CXR and Echo
Daily urine dipstick for protein, ME and C&S –
every morning
Daily BP, weight and abdominal girth
Start on IV infusion
Administration of IV albumin
Start on steroid therapy – prednisolone given at
a dose of 2mg/kg/day divided into 2-3 doses.
This regimen is continued until remission is
achieved
Remission is achieved when the urine is 0 or
trace for protein for 5 to 7 consecutive days
Administer prophylactic antibiotics to reduce
infections
Start on diuretic therapy – frusemide (lasix)
Dietary restriction – provide ↑ protein, high
carbohydrate, ↑ potassium diet & no salt diet
Strict I/O chart
Provide careful skin care
Good hygiene
CRIB
Question and Answer
DEFINITION
The backflow or reflux of urine from the
bladder into the ureters and possibly the
kidneys. The urine returns to the bladder after
passing urine.
Fever >39ºC
Irritability
Poor feeding
Vomiting
Dysuria as evidenced by crying when passing
urine
Change in urine colour or odor
Abdominal or suprapubic pain
Frequency in passing urine
Urgency in passing urine
Dysuria
New or increased incidence of
enuresis
In normal functioning urinary tract, there is
a valve-like mechanism at the junction of
the ureter and bladder that prevents urine
from refluxing in the ureters
As urine fills the bladder or the bladder
contracts during micturating, pressure in
the bladder occludes the opening to the
ureter
When a defect occur at the vesioco-ureteral
junction, VUR occur
MCUG – to visualise the urethra, evaluate
degree of reflux and define any
abnormalities
Renal scan – to assess renal scarring and
function
Urodynamic studies – this is done when
there is micturating dysfunction (frequency,
urgency, or incontinence) is present
Cystograms
Urine culture
Blood test – serum creatinine
GRADE I: reflux into ureter only – no
dilatation
GRADE II: reflux into ureter, pelvis and
calyces with no dilaltation and normal
calyceal fornices
GRADE III: mild dilatation of ureter and renal
pelvis
GRADE IV: moderate dilatation of ureter,
pelvis and calyces
GRADE V: gross dilatation of ureter, pelvis
and calyces
GRADE IV:
moderate dilatation
of ureter,
pelvis and calyces
GRADE V:
gross dilatation
of ureter,
pelvis and calyces
Reflux can be divided into 2 categories :1.
PRIMARY REFLUX
- caused by abnormal position of the
ureteral bud on the wolffian duct during
development of the urinary tract, resulting
in smaller, tunneled segment of the ureter
2.
SECONDARY REFLUX
- occurs as a result of acquired bladder
dysfunction
Daily low dose of prophylactic antibiotic to
prevent UTI
Urinalysis and urine ME/CS – every 3 to 4
months to evaluate for UTI
Monitor ↑BP
Surgery – reimplantation of the ureter into the
bladder
Indicated due to recurrent UTI despite
antibiotics, Grade 5 reflux or progressive renal
injury
Definition
Hypospadias is a congenital
anomaly in which the actual
opening of the urethral meatus is
“below” the normal placement on
the glans of penis
Occurs from incomplete development of the
urethra in utero
Exact causes unknown – may be genetic,
environmental or hormonal factor
Stenosis of the opening could occur – may lead
to UTI or hydronephrosis
May interfere with fertility if left uncorrected
The location of the meatus may make it difficult
for the child to urinate standing up
The choice of surgical correction is affected
primarily by the severity of the defect
Surgery is done when the child’s age is less
than 18 months
Reconstruction of the meatal opening is done –
Meatal advancement granuloplasty (MAGPI)
The goal for surgical correction: To enhance the child’s ability to pass urine in
the standing position with a straight stream
To improve the physical appearance of the
genitalia for psychological reasons
To preserve a sexually adequate organ
1.
Ashwill, J.W. and Droske, S. C. 1997. Nursing
Care of Children. Principles and Practice. USA:
W.B. Saunders.
2.
Brunner, L.S. and Suddarth, D.S. 1986. The
Lippincott Manual of Peadiatric Nursing. (3rd
ed.) UK: Chapman & Hall.
The End