Letrozole
advertisement

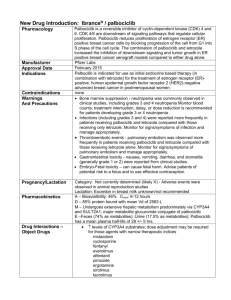
Letrozole versus hMG in intrauterine insemination cycles H. Jamal; H. Serdaroglu; A. Baysoy; E. Karatekeli; E. Attar; H. Ozornek Istanbul, Turkey Aromatase Inhibitors i-Steroid group: Exemestane ii-Non-Steroid imidazole group: Fadrozole. iii-Non-Steroid triazole group: Anastrazole, letrozole letrozole letrozole reversible Increases endogenous production of FSH Suppressing estrogen Enhances ovarian response to gonadotropin stimulation Increasing intraovarian androgen levels Advantages of third-generation aromatase inhibitors Extremely potent inhibition of aromatase Very specific inhibition of aromatase without significant inhibition of other steroidogenesis enzymes Oral administration 100% bioavailability after oral administration Rapid clearance from the body (short half-life, ~ 45 hours) No accumulation of the medications or their metabolites No significant active metabolites Few mild adverse effects with high tolerability when given chronically Few contraindications or drug interactions Relatively inexpensive Indications Breast cancer Endometrial cancer Endometriosis uterine fibroids Ovulation induction a) Unexplained infertility b) PCO c) Poor responders IUI Human reproduction Mitwally et al. 2003 Clinical pregnancy rate 25 20 15 10 19.1% 18.7% 10.5% 5 0 LetrozoleFSH CC-FSH FSH-only IUI Fertility and Sterility Healey et al. 2003 Clinical pregnancy rate 25 20 15 20.9% 21.6% FSH FSH+Letrozole 10 5 0 Objective A prospective randomized study comparing the results of intrauterine insemination (IUI) in women undergoing ovulation induction with either letrozole or Human Menopausal Gonadotropin (hMG). Letrozole group IUI hMG group 80 couples regular menstrual cycles LETROZOLE GROUP(40 CASES) primary infertility hMG GROUP(40 CASES) female age <36 years All patients diagnosed as having unexplained infertility (lack of conception after at least 2 year of regular unprotected intercourse) • Transvaginal ultrasound • Hormone profiles • Semen analysis • Hysterosalpingogram • and/or Laparoscopy normal normal OHSS and multiple pregnancy length of follicular phase clinical pregnancy rate 14 mm follicles premature LH surge endometrial thickness Letrozole & hMG cost LH surge? LH-surge was defined as an increase in LH level ≥100% over mean of preceding two days. Letrozole vs hMG Day 3 HCG Day 7 Letrozole 2x1 Day 3 Day 7 hMG 1x75ıu (<30 years) hMG 1x150ıu(30years) hMG IUI was performed by the same physician for all patients. No luteal support was given. RESULTS Letrozole (n=40) hMG (n=40) 27.22±5.5 28.1±4.3 Duration of infertility (yrs) 5.3±2.1 5.9±3.2 baseline FSH (IU/l) 6.41±2.6 6.11±1.7 baseline LH (IU/l) 4.81±4.5 5.29±2.1 baselin E2 (pg/ml) 39.54±12.0 41.74±13.4 Age (yrs) P: NS RESULTS Semen parameters before preparation for insemination Letrozole hMG [40] [40] Age of male partner (yrs) 31.43±4.1 30.10±5.9 Concentration (x106/ml) 63.9 ± 41.3 66.3 ± 44.4 Motility (%) 59.7 ± 16.1 62.4 ± 15.3 NS Normal sperm forms (%) 52.9 ± 11.3 54.1 ± 9.2 NS P value NS NS RESULTS Letrozole hMG P value 12.77±1.9 11.90±1.7 NS Follicle number 1.79±1.3 3.21±1.6 <0.001 Endometrial thickness(mm) 8.91±1.8 10.05±2.9 NS 93.3% 95.6% NS 193.19±80 875.15±368 <0.001 2 2 NS Follicular phase (days) Trilaminar pattern HCG day E2 Premature luteinization RESULTS Pregnancy rate Multiple pregnancy OHSS Letrozole hMG P value 17.5% 15 % NS 1(triplet) 1(twin) NS 0 1(moderate) NS The mean dose of hMG (mean number of ampoules/cycle) was 15.5 ampoules/cycle. While the dose of letrozole were stable (10 tablets/cycle). Letrozole had a cost of 43 $ per cycle while hMG was more costly with 225 $ per cycle. Conclusion • Although low estradiol levels and less number of mature follicles were obtained at the time of the hCG in the letrozole group, pregnancy rates were similar in both groups. Conclusion • Another outcome we noticed that the stimulation time lasted longer in the letrozole group. As other authors cited before that this longer time of stimulation may have beneficial effects on oocyte maturation and oocyte quality and this is maybe a reason that more pregnancies occured in the letrozole group. Conclusion • Despite significantly lower E2 levels in the letrozole-treated women, endometrial development was unaffected, endometrial thickness and pattern were similar in both groups. Conclusion • Serious complications (OHSS, multiple pregnancy) were rare in the two groups. Low estradiol levels and less number of mature follicles at the time of the hCG in the letrozole group may be a reason to minimize and thereby avoid the complications of ovarian hyperstimulation syndrome (OHSS) and multiple pregnancy. But to compare such an outcome, a large study including a very large number of patients must be required. letrozole efficient cost effective simple and convenient Thanks!