BLEEDING PER RECTUM IN
CHILDREN SURGICAL CAUSES
AND MANAGEMENT
DR NANDLAL KELLA
ASSOCIATE PROFESSOR AND
CHAIRMAN
DEPT; OF PEDIATRIC SURGERY
LUMHS JAMSHORO
Mommy, the toilet’s red!!
DR NANDLAL KELLA
ASSOCIATE PROFESSOR AND CHAIRMAN
DEPT; OF PEDIATRIC SURGERY
LUMHS JAMSHORO
Objectives
•
Definitions
• Common causes of GI bleeding in
•
different age group
Differential Diagnoses
Diagnostic and therapeutic approach
diagnostic and therapeutic approach to the pediatric patient with GI
bleeding
• Review the most common etiologies for GI bleeding in
pediatric patients in various age groups
Important Definitions
Hematochezia – passage of bright or dark red
blood per rectum
• in general, the redder the blood, the more distal the site
of bleeding
Melena – the passage of black, tarry stools
• indicates likely UGI bleed (proximal to the ileocaecal
valve)
Hemetemesis – vomitus containing frank blood or
brown-black “coffee grounds”(proximal to ligament of
Treitz)
Further assessment
• Is it really blood?
– Hemoccult stool, gastroccult emesis
• Apt-Downey test in neonates
• Nasogastric aspiration and lavage
– Clear lavage makes bleeding proximal to ligament
of Treitz unlikely
– Coffee grounds that clear suggest bleeding stopped
– Coffee grounds and fresh blood mean an active
upper GI tract source
Substances that deceive
• Red discoloration
– candy, fruit punch, Jell-o, beets, watermelon,
laxatives, phenytoin, rifampin
• Black discoloration
– bismuth, activated charcoal, iron, spinach,
blueberries, licorice
History
• Present illness
– duration of bleeding , Quality of bleeding ))fresh,
clotted or mixed) or quantity of bleeding
– associated GI symptoms (vomiting, diarrhea, pain)
• Review of systems
– GI disorders, liver disease, bleeding diatheses
– medications (NSAID’s, warfarin)
• Family history :hemophilia or other bleeding disorder
History
•
•
•
•
•
•
•
In newborn
We have to focus mode of delivery
Laboured delivered
Meconeum aspiration
Severe respiratory distress
Trauma
Sepsis/shock
Physical examination
• Vital signs, including orthostatics
• Skin: pallor, jaundice, ecchymoses, abnormal
blood vessels, hydration, cap refill
• ENT: nasopharyngeal injection, oozing;
tonsillar enlargement, bleeding
• Abdomen: organomegaly, tenderness, ascites,
caput medusa
• Perineum: fissure, fistula, induration
• Rectum: gross blood, melena, tenderness
Gastrointestinal Bleeding
• Blood streaks on the stool indicates anal outlet
bleeding
• Blood mixed with stool indicates bleeding source
higher than the rectum
• Blood with mucus indicates an infectious or
inflammatory disease
• Currant jelly-like material indicates vascular
congestion and hyperemia (intussusception or midgut
volvulus)
DDx: neonates
• Upper GI bleeding
– swallowed maternal
blood
– stress ulcers, gastritis
– duplication cyst
– vascular malformations
– vitamin K deficiency
– hemophilia
– maternal ITP
– maternal NSAID use
• Lower GI bleeding
–
–
–
–
–
swallowed maternal blood
dietary protein intolerance
infectious colitis
necrotizing enterocolitis
Hirschsprung’s
enterocolitis
– duplication cyst
– coagulopathy
– vascular malformations
Presentation and Management in
newborn in bleeding
•
•
•
•
•
•
•
presentation
S/s of sepsis
Respiratory distress
Distension of abdomen
Shock
Hypothermia
Hypoglycemia
• Diagnosis
• Clinical Examination
• Investigations;
•
CBC, PT APTT Calcium
• Level ,Glucose level,
• Urea Creatinine and
blood
• C/S
• Ultrasound and X-Rays
Management
•
•
•
•
•
•
•
•
Temp Maintenance
NPO and NG Tube
I/V Fluid
Blood Transfusion
Vit K
Fresh frozen plasma
I/V antibiotics
Oxygen inhalation
• If surgical issue ;
intestinal perforation
After resuscitation
intervention may be
done or patient is very
sick then only peritoneal
cannulation or
catheterization is help
full.
Neonatal stress ulcers or gastritis
• Causes
– Shock
– Sepsis
– Dehydration
– Traumatic delivery
– Severe respiratory distress
– Hypoglycemia
– Cardiac condition
Clinical Findings in PUD
Neonatal Period
• Gastric ulcers are more common than
duodenal ulcers in neonates
• Spontaneous Perforation is a more common
presentation than bleeding
• Frequently associated with:
– Hypoxia, Sepsis, RDS, CNS disorder
DDx: infants
• Hematemesis, melena
– Esophagitis
– Gastritis
– Duodenitis
• Hematochezia
–
–
–
–
–
–
–
Anal fissures
Intussusception
Infectious colitis
Dietary protein intol.
Meckel’s diverticulum
Duplication cyst
Vascular malformation
DDx: children
• Upper GI bleeding
–
–
–
–
–
–
Esophagitis
Gastritis
Peptic ulcer disease
Mallory-Weiss tears
Esophageal varices
Pill ulcers
• Lower GI bleeding
–
–
–
–
–
–
–
–
–
Anal fissures
Infectious colitis
Polyps and prolapse
Lymphoid nodular
hyperplasia
IBD
HSP
Intussusception
Meckel’s diverticulum
HUS
Upper GI Bleeding
<2 Mo
Swallowed maternal blood
Stress ulcer
Vascular malformation
Hemorrhagic disease of newborn
(vitamin K deficiency)
Coagulopathy/bleeding diathesis
2 Mo–2 Y
Gastroenteritis
Toxic ingestion
Mallory-Weiss
tear
Vascular
malformation
Esophagitis
Stress ulcer
Bleeding
diathesis
GI duplication
Foreign body
>2 Y
Gastroenteritis
Mallory-Weiss
tear
Peptic ulcer
disease
Toxic ingestion
Vascular
malformation
Gastritis
Varices
Hematobilia
Foreign body
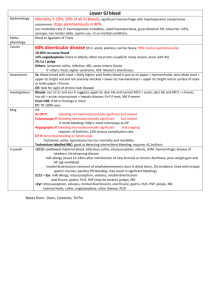
Lower GI Bleeding
<2 Mo
Swallowed maternal
blood
Milk allergy
Infectious colitis
Intussusception
Volvulus
Meckel diverticulum
Necrotizing enterocolitis
Vascular malformation
Hemorrhagic disease of
newborn
Hirschsprung disease
Congenital duplications
2 Mo–2 Y
Anal fissure
Gastroenteritis
Milk allergy
Intussusception
Volvulus
Meckel diverticulum
Hemolytic uremic
syndrome
Henoch-Schönlein
purpura
Polyps; benign,
familial
Inflammatory bowel
disease
GI duplication
>2 Y
Anal fissure
Gastroenteritis
Polyps
Colitis (infectious,
ischemic)
Meckel diverticulum
Intussusception
Hemolytic uremic
syndrome
Henoch-Schönlein
purpura
Inflammatory bowel
disease
Angiodysplasia
Celiac disease
Rectal ulcer
syndrome
Peptic ulcer disease
Clinical Findings in PUD
Infants and Toddlers
• Presenting symptoms:
– Vomiting
– Poor feeding
– Irritability during and after eating
– Abdominal distention
– Hematemesis, melena
• Commonly associated with underlying disease
in this age group
Clinical Findings in PUD
Pre-Schoolers
•
•
•
•
Periumbilical or generalized abdominal pain
Vomiting after eating
Nocturnal or early morning pain
Gastric ulcers are as common as duodenal
ulcers
• Primary ulcers are as common as secondary
ulcers
Clinical Findings in PUD
School Age
•
•
•
•
•
Male: Female ratio is 3:1
Burning epigastric pain
Nocturnal pain
Melena, hematemesis, fecal occult blood
Primary ulcers are more common than
secondary ulcers
Anal Causes
•
•
•
•
Hemorrhoids
Fissure
Perianal abscess/ fissure
Anal carcinoma
Hemorrhoids
• Usually uncommon in children
• Usually benign
• When seen, must suspect portal
hypertension
• Avoidance of chronic constipation, fecal
impaction or other irritating local factors
Anal Fissure
• Small laceration of the mucocutaneous
junction of the anus.
• Acquired lesion secondary to the forceful
passage of a hard stool, mainly seen in
infancy.
• Fissures appear to be the consequence and
not the cause of constipation.
Anal Fissure
Acute posterior anal fissure producing pain on digital exam.
Sphincter tone increased. Exam limited by pain that may
respond to NTG and Lidocaine.
Anal Fissure
• Usually a history of constipation is elicited.
• painful bowel movement
• Patient retains the stool voluntarily to avoid
a painful bowel movement
• Bright red blood on the surface of the stool
Anal Fissure
• Inspection of the Anal area
• Infant’s hips are put in acute flexion
• Buttocks are separated to expand the folds
of the perianal skin
• Fissure becomes evident as a minor
laceration
Anal Fissure
• The most important element in the treatment
is for the parents to understand the origin of
the laceration and the mechanism of the
cycle of constipation.
• Goal of the treatment : REVERSE the
CYCLE
• soft stools to avoid overstretching
Anal Fissure
•
•
•
•
Stool softener
Avoid hard stools and diarrhea
Treat the primary cause of constipation
Local application of pain killer
Anal Fissures in older children
1. A linear tear in the skin of the anal canal caused by passage of a
hard stool, diarrhea, straining, sitting too long. May be seen in IBD
or after rectal surgery. Increased sphincter tone.
2. Deep fissures expose underlying internal sphincter, white color.
3. Spasm, irritation, itching, pain after BM, and bleeding.
4. Acute fissures may heal with sitz baths, fiber, brief Rx steroid
cream, leading to thin skin and sentinel pile. Pile may shrink after
Rx. If persists may be excised after Rx of fissure completed.
5. Associated hemorrhoids are common.
6. NTG, Lidocaine ointment, fiber, fluids, no straining, banding.
7. Infected fissures Rx Flagyl.
Anal Fissure Rx
• 6 weeks of twice a day intra-rectal NTG ointment, .12%, then 6
weeks of once a day NTG. Watch for headaches, tachycardia, or
light headiness. needed.
• 2 % Diltiazem, calcium channel blocker. ointment is an alternative
in those with headaches and is used three time per day and may
take longer.
• Botox effectively paralyzes internal sphincter but costs $600 per
vial and may cause incontinence. May be used in combination with
NTG.
• Surgery is effective but has a 10% incontinence rate.
Skin tags
Skin tags are extra folds of skin around the
anal verge. Caused by stretching of skin from
dilated external hemorrhoids. May interfere
with cleaning and add to pruritus ani. Cosmetic
issue to some.
Skin tag and can be removed or left alone
depending on preference.
Removal requires local anesthesia and office
excision. Takes 15 minutes and leads to 2-3
days of discomfort.
Associated skin tags
Colon Polyps
• The term polyp of the colon refers to a
protuberance into the lumen from the
normally flat colonic mucosa.
• Polyps are usually asymptomatic but may
ulcerate and bleed, cause tenesmus if in
the rectum,.
Colon Polyps
•
•
•
•
Neoplastic (adenomas and carcinomas),
Hamartomatous,
Non-neoplastic, and
Submucosal (neoplastic / non-neoplastic).
Non-neoplastic polyps
•
•
•
•
Hyperplastic
Mucosal
Inflammatory pseudopolyps
Submucosal
Juvenile Polyps
• Juvenile polyps are hamartomatous
lesions that consist of a lamina propria
and dilated cystic glands rather than
increased numbers of epithelial cells
Juvenile Polyp
• May be single or a few, located throughout the colon; virtually always
benign
• Occasionally multiple (juvenile poyposis coli)
o In JPC, may have potential for adenomatous change
• Diagnosis: Colonoscopy
• Treatment: Endoscopic Polypectomy
Juvenile colonic polyp
Familial Juvenile Polyposis
• FJP is associated with an increased risk
for the development of colorectal cancer,
and in some families, gastric cancer,
especially where there are both upper and
lower gastrointestinal polyps.
Diagnosis and Treatment
• Diagnosis almost always is made at digital
rectal examination.
• Double contrast barium enema is not
suggested
• Endoscopy for diagnostic as well for
therapeutic
• Polyps biopsy necessary to exclude
malignancy
Rectal prolapse
Definition
• Protrusion of few or all layers of rectal wall
through anal sphincter
Etiology
•
•
•
•
•
•
Constipation
Diarrhoea
Parasites
Neuro muscular and pelvic disorders
Malnutrition
Surgical causes ARM Cloacal exstrophy
Presentation
• Prolapse of rectum
• Incontinence of stool
• Bleeding from prolapse
management
•
•
•
•
•
•
Treat the cause
Pushing back of prolapsed rectum
Decrease straining
Laxatives and stool softener
High protein diet
Rarely surgery or sclerotherpy
What is Meckel’s
• A Meckel's diverticulum is a small bulge in the
small intestine present at birth
• It is a vestigial remnant of the
omphalomesenteric duct, and is the most
frequent malformation of the gastrointestinal
tract
• It is present in approximately 2% of the
population, found twice as frequently in males
as females, although males more frequently
experience symptoms
• It is named after Johann Friedrich Meckel, who
first described this type of diverticulum in 1809
What is Meckel’s
• It can usually be found within about 60100 cm of the ileocecal valve. It is
typically 3-5 cm long, runs
antimesenterically and has its own
blood supply
Symptoms of Meckel’s
•
Approximately 98% of people afflicted with Meckel's diverticulum
are asymptomatic. If symptoms do occur, they typically appear
before the age of two.
•
The most common presenting symptom is painless rectal
bleeding, followed by intestinal obstruction, volvulus and
intussusception.
•
Occasionally, Meckel's diverticulitis may present with all the
features of acute appendicitis. Also, severe pain in the upper
abdomen is experienced by the patient along with bloating of the
stomach region.
•
At times, the symptoms are so painful such that they may cause
sleepless nights with extreme pain in the abdominal area.
Diagnosing Meckel’s
• OTHER CONSIDERATIONS/RATIONALE:
– The radiopharmaceutical is actively secreted by
gastric mucosa. Although all Meckel's diverticula
do not contain functioning gastric mucosa, most
that bleed do
– Patient's with active hemorrhage can also be
studied with tagged red blood cells. While only
20% of Meckel's Diverticula contain ectopic
mucosa, greater than 90% of diverticula that bleed
do.
Meckel Scan
• Technetium-99pertechnetate
• Concentrates in gastric
mucosa
• Premedicate with H2
blocker to enhance uptake
and minimize risk of
stomach or bleeding
obscuring the diverticulum
• Can also identify
duplications
ONLY 50% OF PROVEN
MECKEL’S HAVE A POSITIVE
SCAN
FIGURE 59.8. Meckel Diverticulum. A small focus (arrow) of technetium-99pertechnetate uptake gradually becomes visible in the ectopic gastric mucosa of
a Meckel diverticulum in the midabdomen.
http://www.msdlatinamerica.com/ebooks/FundamentalsofDiagnosticRadiology/sid613328.html
Treatment of Meckle’s
• Treatment is surgical, consisting of a resection of
the affected portion of the bowel.
INTUSSUSCEPTION
DEFINITION
Telescoping
of a proximal segment of
the intestine (intussusceptum) into a
distal segment (intussuscipiens)
Intussusception: invagination of one segment
of intestine into another segment
Ileocolic intussusception
INTUSSUSCEPTION
EPIDEMIOLOGY
Incidence 2 - 4 / 1000 live births
Usual age group 3 months - 3 years
Greatest incidence 6-12 months
Male predominance (1.5-2 : 1)
No clear hereditary association
No seasonal distribution
Frequently preceded by viral infection
Second most common cause of acute abdominal pain
in children following appendicitis
Why does Intussusception
happen?
Idiopathic 60%
Most are ileocolic
Lead point <10%
•Most common is Meckel’s diverticulum
•Other possibilities include : polyps, hemangiomas,
lymphomas, cysts, buried appendix, parasites, cystic
fibrosis and HSP
•American and European studies showing <10% of cases
having a lead point
More common post-surgery patients
Hypotheses of etiologies:
INTUSSUSCEPTION
ANATOMIC LOCATIONS
ILEOCOLIC
– MOST COMMON IN CHILDREN
ILEO-ILEOCOLIC
– SECOND MOST COMMON
ENTEROENTERIC
– ILEO-ILEAL, JEJUNO-JEJUNAL
– MORE COMMON IN ADULTS
– MAY NOT BE SEEN ON BARIUM ENEMA
CAECOCOLIC, COLOCOLIC
– MORE COMMON IN AFRICAN CHILDREN
Pathophysiology
invagination of the bowel
Obstruction resulting in compression
of the vessels and venous congestion
and bowel wall edema
Infarction,
perforation
If left untreated, FATAL
Classic Triad
Colicky
abdominal pain
“Currant Jelly” bloody stools Abdominal Mass
-sausage shaped
-pulling knees up to abdomen
•Multiple studies have shown that classic triad is only present in 2
•70% found to have 2 symptoms
•9% found to have 1 symptom
Differential diagnosis of
bleeding per rectum
Dysentery
Bleeding disorder
Sepsis/DIC
Malrotation
Volvulous
Rectal polyp
Fissure/ rectal prolapse
Diagnosis
The longer you take to diagnose, the
higher the probability of surgery and
mortality
Diagnosis made by clinical presentation
and imaging
However, clinical suspicion can guide the
modality of imaging…
Abdominal X-Ray
Conventionally, first-line modality for suspected
intussusception
Low sensitivity, high false negative rate
Can be negative in early IS
Uses:
-Diagnosis of IS
-Evaluating for risk of perforation before enema
treatment
-Diagnosis of other diseases (Small BO, Large
BO, volvulus)
•Findings:
1) Intracolonic mass
Where is
the target
sign?
Created by
gas trapped
between
two layers
of intestinal
wall
Where is
the
crescent
sign?
Created by gas
surrounding
invagination
Gas in RLQ?
There is
dilation of
LUQ, but no
presence of
gas anywhere
else in the
bowel.
Ultrasound
•Used to diagnose IS and prevent unnecessary enemas
High sensitivity and specificity
No radiation exposure
•Findings:
-target sign (transverse)
-pseudokidney or sandwich sign (longitudinal)
Treatment
17% of IS spontaneously reduce
1st – NPO, IV fluids, NG tube
2nd – surgery consult
Otherwise, tx by reduction enemas or surgery
Reduction Enema •Indications –
•Successful when
irreducible by enema,
flow moves into ileumnecrotic IS, age, long
•Pt is under sedation duration of sx, SBO,
•Disadvantages –
or clinical signs/sx of
missed lead points, peritonitis or bowel
higher recurrence
infarction
rate, perforation, and
radiation exposure
Surgical Emergencies with Lower GI
Bleeding
Hirschprung’s
• Bloody stool portends
enterocolitis
• May be mimicked by
severe GI allergy
Malrotation and Volvulus
Imaging studies and indications
• Upper GI series: dysphagia, odynophagia,
drooling
• Barium enema: intussusception, stricture
• Abdominal US: portal hypertension
• Meckel’s scan: Meckel’s diverticulum
• Sulfur colloid scan, labeled RBC scan,
angiography : obscure GI bleeding
Endoscopy: indications
•
•
•
•
EGD: hematemesis, melena
Flexible sigmoidoscopy: hematochezia
Colonoscopy: hematochezia
Enteroscopy: obscure GI blood loss
Esophageal varices
The Likely Causes of GI Bleeding
Differ at Varying Ages
Infectious Enterocolitis
• Bacterial infections
o
o
Salmonella, Shigella, Campylobacter, E coli
C. difficile – may not have clearcut history of
antibiotic exposure
• Viral infections - only CMV in the
immunocompromised host
• Parasitic - amebiasis
Inflammatory Bowel Disease
• Both Crohn’s and UC can present with
bloody diarrhea
• Exclude infectious causes before initiating
invasive diagnostic procedures
o
CT evidence of diffuse or segmental bowel
inflammation does not preclude an infectious
etiology
Proctitis/Proctosigmoiditis
• Most common presentation of colitis in adults
• Typically, painless hematochezia is only symptom
o
Tenesmus often mistaken for constipation
• Laboratory evaluation often entirely normal
Anal Lesions
External hemorrhoids
Crohn’s anal tags
• Hemorrhoids are extremely uncommon in the
child and adolescent
• Fleshy rather than vascular lesions should raise
the suspicion of Crohn’s disease
Milk Protein Allergy
• Presentations
o
Hematochezia – usually in first 3 months of life
Diarrhea, irritability, ± poor weight gain
o
o
Hypoalbuminemia, anasarca
“GE reflux”
• Labs
o
o
Variable eosinophilia in blood and biopsy
Skin prick, RAST testing negative
• Treatment
o
Casein hydrolysate or amino acid based formula
Esophageal Varices
Vascular Anatomy of Portal Hypertension
www.bio.ri.ccf.org
Portal Hypertension
• Intrahepatic (e.g. cirrhosis)
• Post-sinusoidal
o
Budd Chiari syndrome (hepatic vein thrombosis)
• Presinusoidal
o
o
Splenic vein thrombosis
Cavernous transformation of the portal vein
Endoscopic Therapy for Varices
Sclerotherapy
Band Ligation