Epistaxis - Mededcoventry.com
advertisement

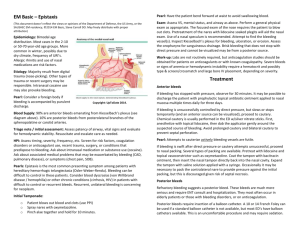
Very common Usually self limiting Rarely massive bleeding can be fatal To understand the causes and predisposing factors To consider assessment and management To review complications Is bleeding from the nose caused by damage to blood vessels of nasal mucosa Anterior (80-90%), Little’s area anterior nasal septum – Keisselbach plexus of vessels Posterior from branches of sphenopalatine artery in posterior nasal cavity 60% of population 6% seek medical attention Peaks – 2-10 years greater than 45 years – posterior epistaxis more common in older people Under 2 years rare and may be associated with injury or underlying serious illness Nosepicking Nasal fractures Septal ulcers / perforation Foreign body Blunt trauma e.g. falls Infection Allergic rhinosinusitis Nasal polyps Topical drugs-cocaine, nasal decongestants Vascular –hereditary haemorrhagic telangiectasia Wegeners granulomatosis Post-operative – ENT, max fax, ophthalmic Benign tumours – angiofibroma Malignant tumours – squamous cell Nasal oxygen Hypertension Atherosclerosis Increased venous pressure from mitral stenosis Alcohol Environmental – temperature, humidity, altitude Thrombocytopaenia Platelet dysfunction Leukaemia Haemophilia Anticoagulant drugs Antiplatelet drugs e.g aspirin, clopidogrel Most self-limiting and do not require medical treatment Transfusion unusual Massive bleeding rare but can be fatal ABC resuscitation as required Lean forward (decreases blood flow through nasopharynx) Open mouth, spit blood into bowl, minimises swallowing Pinch soft part of nose for 10-15 minutes CONTINUOUSLY Duration Which nostril Estimated blood loss Any home management / packing Previous epistaxis and management PMH –likely underlying causes Surgery Trauma Symptoms suggestive of tumour ◦ ◦ ◦ ◦ Nasal obstruction Rhinorrhoea Facial pain Facial numbness, double vision Drugs FH bleeding disorders environmental ABC General examination Local examination Light source and nasal speculum Get patient to blow nose ( dark blood or clots likely to be old) Look for bleeding point ( if bleeding stopped , small red dot < 1mm) Profuse bleeding from both nostrils with no visible bleeding point on speculum examination suggests posterior bleed FBC if heavy or recurrent bleeding or clinically anaemic (often not required) Coagulation – if on warfarin or bleeding diathesis suspected Group and save / cross match - if bleeding heavy, shock, severe anaemia Naseptin (chlorhexidine and neomycin) qds for 10 days Avoid in peanut allergy – use mupirocin instead Reduces crusting and vestibulitis Very useful in young children as cautery inappropriate Use if first aid unsuccessful, not for young children Need appropriate expertise and equipment Blow nose Anaesthetic spray preferably with vasoconstrictor (eg lignocaine and phenylephrine) Allow 3-4 mins for anaesthetic to work Identify bleeding point Apply silver nitrate stick to bleeding point for 3-10 seconds until grey-white colour develops Only one side of septum to avoid septal perforation Avoid touching area not requiring treatment Dab cauterised area with clean cotton bud to remove chemical or blood Naseptin or mupirocin cream Self care advice Avoid blowing or picking nose Avoid heavy lifting Avoid strenuous exercise Avoid lying flat Avoid alcohol and hot drinks ( cause vasodilation) If further bleeding unresponsive to first aid measures, return to ED If bleeding not controlled Local anaesthetic and vasoconstrictor Nasal tampon (merocel) Inflatable packs (rapid rhino) Impregnated ribbon gauze – needs specific expertise Position sitting forward mouth open Secure pack to cheek Check no pressure on cartilage around nostril Check oropharynx for bleeding, may need to pack both nostrils Admit ENT Sinusitis Septal haematoma /abscess (from traumatic packing) Pressure necrosis (from excessively tight packing) Toxic shock syndrome (prolonged packing) Airway obstruction Uncontrolled bleeding Posterior bleeding Nasal pack Significant comorbidities clotting disorder, anaemia Recurrent with high risk of underlying cause Formal packing Endoscopy and electrocautery EUA and surgical intervention e.g. Arterial ligation Radiological arterial embolisation IV or oral tranexamic acid History and examination Consider underlying cause Refer children under 2 years for further investigation Manage with topical antiseptic or nasal cautery Refer if epistaxis not settled or high risk of serious underlying cause Reference – NICE 2010 ABC and resuscitation plus first aid measures History – and consideration of underlying cause Examination local /general Investigation where appropriate Management Referral to ENT