uppergiemergencies - Global Emergency Health Medicine
advertisement

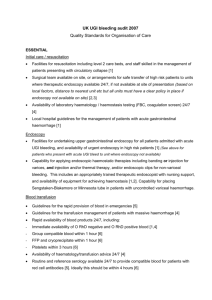
Upper Gastrointestinal Emergencies Author: Andrew McDonald MD, FRCP, Assistant Professor Date Created: January 2012 Global Health Emergency Medicine Teaching Modules by GHEM is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. Learning Objectives Understand the approach to GI bleeding Understand the approach to esophageal injuries from caustics and foreign bodies Understand the approach to peptic ulcer disease and gastritis Case example A 31 year old man is brought by his family after vomiting black material for two days He appears unwell and lethargic HR 130 BP 90/50 RR 30 T 35°C Family says he has a history of chronic liver disease GI bleeding – How patients present History of vomiting blood or rectal blood Shock +/- passing blood Decreased LOC +/- passing blood Challenges in these patients Management of hypovolemic shock Vomiting and aspiration Hepatic encephalopathy Coagulation disorder Causes of Upper GI bleeding Peptic ulcer disease Gastritis Varices Mallory – Weiss tear rare Malignancies Causes of Lower GI bleeding Hemorrhoids Diverticulosis Malignancies/polyps Angiodysplasia (AVM) of aging Inflammatory bowel disease Complications of Typhoid fever Upper GI bleeding Bloody diarrhea Epidemiology Little is documented on the epidemiology of GI bleeding in developing countries Clinical features Hematemesis = upper GI source Hematochezia = lower GI source Melena = don’t know source Clinical features (continued) Weight loss -- Think of malignancy Bleeding following vomiting -- Think of Mallory Weiss tear Medications can cause bleeding: NSAID/ASA Steroids Anticoagulants Alcohol use/abuse associated with various types of bleeding Clinical features (continued) Establish vascular volume status Confirm bleeding by site Do a rectal exam to look for bright red blood or melena; perform a guaiac test if available Role for NG tube? Look for signs of liver disease Look for generalized bleeding problem Management Assess for airway management Prompt large bore iv access Volume resuscitation if necessary as patients can deteriorate rapidly CBC, cross match, LFT, coagulation, renal Reverse any coagulopthy if possible Access to endoscopy as diagnostic and therapeutic procedure (Ideal <24 hours) Management (cont.) - Medications Reducing gastric acidity via H2 blockers or PPI meds Reducing portal pressure for varices Antibiotics may improve survival Use of Sengstaken-Blakemore tube not recommended due to complications Need for surgery uncommon Case continued Patient’s airway reflexes were intact Given Oxygen for shock state Monitored vascular/respiratory status closely Administered fluids to improve perfusion Cross matched for blood and plasma to restore hemoglobin and coagulation PPI and antibiotics given while waiting for endoscopy Esophageal Emergencies Esophageal emergencies Causes: Varices Ingestion of corrosives Foreign bodies Caustics – how patients present Pain Difficulty swallowing Airway compromise Challenges in these patients Protecting healthcare workers Pain masking complications Systemic effects of chemical/co-ingestion Mental health issues Causes Intentional self harm versus accidental Sources of chemical information Causes (continued) Alkali – liquefaction necrosis, thrombosis Acids – coagulation necrosis, eschar, systemic absorption Clinical features Pain – range of severity Respiratory/airway symptoms GI symptoms Absence of oral injury does not preclude GI injury! Management Protect yourself Airway assessment – direct vision technique Treat shock = GI bleed, perforation, delayed sepsis, metabolic Decontaminate eyes and skin as needed Surgical consult if perforation Esophageal FB – How patients present Usually based on history Chest pain, retching, can’t swallow Beware of children, mental health, “prisoners” Clinical features Problems with handling secretions Location in esophagus Pediatric typically proximal Adults typically distal Perforation is uncommon Endoscopy is diagnostic and therapeutic procedure Diagnosis X-ray can show the location of a foreign body Management Endoscopy preferred Time +/- sedation often works Meds: Glucagon 1 mg IV Nifedipine 10 mg SL Nitroglycerine SL Management (continued) Button batteries and coins: Remove if in esophagus if endoscopy available Remove if still in stomach after 24 h Sharp objects Endoscopy preferred if available Ulcers and Gastritis Ulcers and gastritis – How patients present Pain GI bleeding Perforation (shock) Causes H. pylori infection Meds: NSAID/ASA Alcohol Spices Severe physiological stress Clinical features Pain Often epigastric tenderness without peritonitis Tests not really useful except to rule out other things Management Perforation, bleeding discussed elsewhere Antacids H2 blockers, PPI Antibiotic therapy Avoidance of NSAID and alcohol Quiz Quiz Question 1 Which is the most common cause of upper GI bleeding? A. B. C. D. Malignancy Intestinal perforation Peptic ulcers/gastritis Mallory Weis tear Quiz Question 2 GI bleeding can present as: A. B. C. D. E. Melena Hematemesis Shock without obvious blood loss Hematochezia All of the above are correct Quiz Question 3 In managing patient after a caustic ingestion: A. B. C. D. They usually present with shock Those without any pain are the sickest Their vomit can be harmful to care givers An NG tube should always be placed Quiz Question 4 Regarding esophageal obstruction: A. Endoscopy is never indicated B. If batteries are not obstructing the esophagus, they can be left there for up to three days C. Adults and children usually obstruct proximally D. All patients with obstruction should be intubated E. Medications may sometimes prevent the need for endoscopy Quiz Question 5 Regarding patients with peptic ulcer disease: A. B. C. D. Abdominal pain is usually constant Alcohol use is one of the causes of ulcers Acetaminophen is a common cause of ulcers The usual treatment is surgical repair Summary GI bleeding can be a cause of lifethreatening shock requiring resuscitation Esophageal injuries should be managed in conjunction with endoscopy experts Peptic ulcer disease and gastritis can present as life-threatening complications General References Tintinalli, JE et al (2011) Chapters 78, 79, 80, 81, 194. McGraw Hill Publishers Emergency Medicine – A study guide 7th Edition, USA Manson’s Tropical Diseases, Chapter 10. Saunders Elsevier, 22nd edition.