fluoroquinolone
advertisement
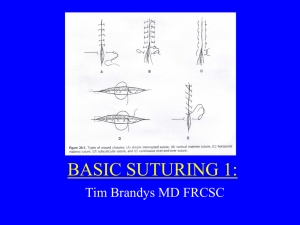
LACERATIONS OF THE LEG AND FOOT BY S. SUPALERK Introduction • Any injury to the lower extremity (especially the foot ) jeopardizes the ability to walk • From simple plantar puncture wounds to catastrophic lawn mower injuries • Soil contamination , risk of infection , worsening scarring , slowing healing Clinical features • History – Time interval : increase incidence of infection – Mechanism of injury : underling tissue – Risk of retained foreign body – Degree of potential contamination – Complaint any new paresthesia , anesthesia weakness or loss of function suggests a nerve vascular or tendon injury prompting a careful examination • Past medical history – Tetanus immunization status – Condition increase risk for infection or delayed wound healing ( DM , immunosuppression ) and risk of bacteremia ( valvular heart disease , asplenia ) – Other medication Physical examination • • • • • • • • Location Length Depth Shape of wound Weight bearing surface Distal sensory nerve function Motor function Vascular integrity • Nerve : light touch , static two-point discrimination – Superficial peroneal N. : foot eversion – Deep peroneal N. : foot inversion , ankle dorsiflexion – Posterior tibial N. : ankle plantar flexion • Tendon : direct visual because partially lacerated tendon can mimic normal fuction • Foreign bodies Ancillary studies • • • • CBC ESR CRP H/C • Radiographic imaging – Foreign body – Fracture – Joint space • CT • MRI Treatment Age considerations • Elderly – thin skin , decrease subcutaneous fat – Medical condition : delay wound healing – Tetanus immunization • Child – Difficulty limit movement – Contaminated wound – The smaller the child, the larger the dressing Wound anesthesia • Sensory examination precede anesthesia • Dorsum foot , local anesthesia • Plantar surface , nerve blocks (sural , posterior tibial ) • Toes , digital nerve blocks • Topical anesthetic poorly effective on dense epidermis Wound preparation and repair • • • • Wound irrigation anesthesia Dry field exploration : tendon , FB LW multiple layered closure decrease tension and simple interrupted , horizontal mattress suture use moderate tension , large LW avoid running sutures , infection • Debridement to remove devitalized tissue decrease risk of wound complication • Timing of closure , delay in closure • Delay primary closure less than 6 hr in case delayed presentation or contamination : pack saline soaked gauze • Antibiotic • reevaluated case Plantar laceration • Pron position • Heavy , large suture needles and thick thread penetrate the hypertrophied epidermis and dermis of foot and sole , large curved cutting needle • Simple interrupted sutures • Tissue loss or under tension use vertical mattress suture • Avoid adhesive tapes , tissue adhesives , staples Dorsal laceration • Nonabsorbable monofilament suture material • Running sutures are acceptable • Under select circumstances adhesive tapes with splints 5-7 days Inter digital laceration • Between toe very difficult to repair • Simple interrupted suture • When the web involve neurovascular , the skin usually closed without any subsequent consideration to repair neurovascular Skin laceration • Wound over the anterior tibial surface are under considerable tension suggest multiple layered closure • Elderly extremely thin and difficulty for closure suggest multiple layered • Elastic bandage is placed over a generous dressing • Weight bearing limited for 5 days • Alternative : deep reinforced sutures placed through adhesive strips laid down parallel to the wound edges has been recently described Knee laceration • Joint capsule penetration , LW of patellar and quadriceps tendons should be assessed • Common peroneal nerve is prone to injury check inversion , eversion , dorsiflexion • Deep popliteal wound : popliteal artery ( minimal collateral circulation distal to knee ) , tibial nerve • Mark active skin tension : knee immobilized Tendon laceration • Repair tendon laceration in foot depend on functional impairment • Tendon at Mid foot and forefoot can go unrepaired ( without sacrificing any necessary foot function ) can close skin and splint • Extensor hallucis longus or tibialis anterior : call orthopedist because dorsiflexion of the great toe and foot important in walking and running • Achilles tendon is first palpated for defects : Thomson test • Repair a few days to weeks after initial injury • Skin closure , splinting of the foot • Antibiotic prophylaxis • Non-weight bearing • Follow up orthopredist Tissue loss and Amputation • Major tissue loss as well as toe amputation • Tissue grafts and flap reconstruction by an orthopedist or plastic surgeon • Serve part : – wash gently with sterile saline – wrapped in saline-soak gauze – placed in plastic bag and closed – placed ice water bath Retained foreign bodies • Nonreactive FB ( glass ) is show chronic pain or chronic discomfort during walk if not removed • Reactive organic material must aggressively sought and removed • Fluoroscopy can use to help locate and remove radiopaque FB Hair tourniquet Syndrome • Strangulation and digital ischemia seen during infancy : long strand of hair wrapped around a toe Disposition • Bulky dressing is applied to plantar surface • Weight-bearing is avoided for at least 5 days • Elevation : decrease swelling and infection risk • Typically removed sutures in 10 – 14 days Prophylactic Antibiotic Use • Clinical adjustment according – Degree of contamination – Presence of foreign body – Presence of associated injury – Host factors Amoxicillin - Clavulanate • Animal bite : staphylococcus , streptococcus , pasteurella • Asplenic or immunocompromised sustain dog bite : C.canimorsus. • Open fractures • S.aureus – First – generation cephalosporin – aminoglycoside fluoroquinolone • Freshwater stream – Aeromonas hydrophila – Gramnegative bacillus Compartment syndrome , myonecrosis , foot amputation • Aminoglycosides • Trimethoprim – sulfamethoxazole • fluoroquinolones