TPTD information - The Royal Berkshire NHS Foundation Trust
Information Sheet
Tibialis Posterior Tendon Dysfunction
Introduction
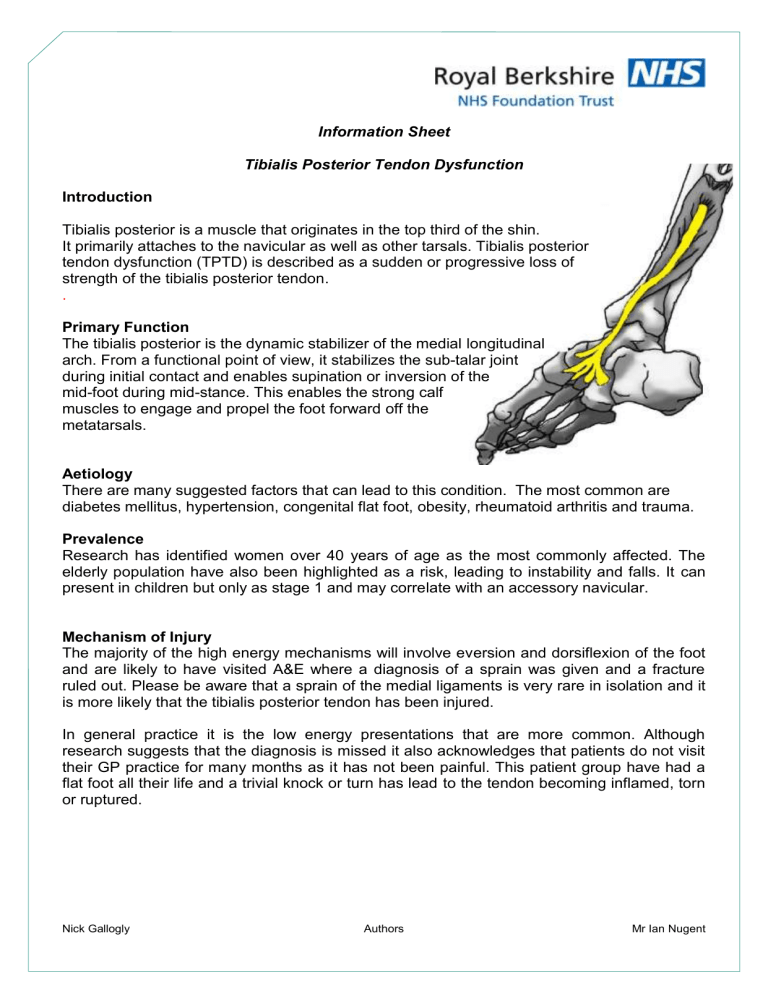
Tibialis posterior is a muscle that originates in the top third of the shin.
It primarily attaches to the navicular as well as other tarsals. Tibialis posterior
. tendon dysfunction (TPTD) is described as a sudden or progressive loss of strength of the tibialis posterior tendon.
Primary Function
The tibialis posterior is the dynamic stabilizer of the medial longitudinal arch. From a functional point of view, it stabilizes the sub-talar joint during initial contact and enables supination or inversion of the mid-foot during mid-stance. This enables the strong calf muscles to engage and propel the foot forward off the metatarsals.
Aetiology
There are many suggested factors that can lead to this condition. The most common are diabetes mellitus, hypertension, congenital flat foot, obesity, rheumatoid arthritis and trauma.
Prevalence
Research has identified women over 40 years of age as the most commonly affected. The elderly population have also been highlighted as a risk, leading to instability and falls. It can present in children but only as stage 1 and may correlate with an accessory navicular.
Mechanism of Injury
The majority of the high energy mechanisms will involve eversion and dorsiflexion of the foot and are likely to have visited A&E where a diagnosis of a sprain was given and a fracture ruled out. Please be aware that a sprain of the medial ligaments is very rare in isolation and it is more likely that the tibialis posterior tendon has been injured.
In general practice it is the low energy presentations that are more common. Although research suggests that the diagnosis is missed it also acknowledges that patients do not visit their GP practice for many months as it has not been painful. This patient group have had a flat foot all their life and a trivial knock or turn has lead to the tendon becoming inflamed, torn or ruptured.
Nick Gallogly Authors Mr Ian Nugent
Assessment
Ensure that both socks and shoes are removed and assess the feet from behind, checking for symmetry. Ask your patient to go onto tip toe. If they are unable to do this or if the heel does not invert, it is likely that a TPTD diagnosis can be given. Symptoms are found around the posterior aspect of the medial malleolus and over the navicular tuberosity where it primarily attaches. Pain and swelling can also be found on the lateral aspect of the ankle where bony impingement has occurred secondary to the excessively pronated posture. TPTD is a clinical diagnosis
Classification
There are four stages to this condition. Please be aware that this condition does progress if left unmanaged
Stage Presentation
1
2
3
The tendon has become dysfunctional and there is now asymmetry in the foot posture. There is pain on the lateral aspect of the ankle and the patient has difficulty or is unable to perform a single heel rise.
The foot deformity has become fixed and there are degenerative changes to the sub-
4
Referral pathway talar joint. There is a significant flat foot deformity.
As stage 3 but degeneration has progressed into the ankle joint
Stage
1
Presentation
Rest, NSAIDs, Supportive footwear advice, Off the shelf insoles +/- physiotherapy input. If unsettled after 6 weeks, refer to the Orthotics department.
2
The tendon is intact and functioning but is painful and inflamed. There is foot symmetry and a single heel rise can be performed. The foot is correctable.
Rest and advice on support footwear with no barefoot walking or slippers. Refer to
Orthotics Department. Refer also to orthopaedic department if the pain is significant.
3 Advise supportive footwear as much as possible and refer to Orthotics department
Please note that should the Orthotist feel that an orthopaedic input is required a letter will be sent to inform you of this .
Imaging
X-rays are not generally required. As the tendon is superficial it can be well detected with an ultrasound. MRI is a useful tool for those that have significant degeneration and are likely to require surgical intervention.
Nick Gallogly Authors Mr Ian Nugent