Pharmacology of the
Endocrine System
Topics
Pituitary and hypothalamic hormones
Thyroid and antithyroid Drugs
Adrenal Drugs
Pancreatic Drugs
Gonadal hormones and inhibitors
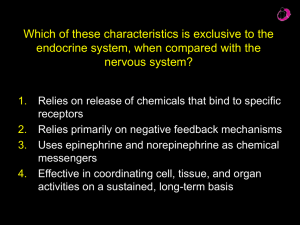
The Endocrine System
Controls many body functions
– exerts control by releasing special chemical
substances into the blood called hormones
– Hormones affect other endocrine glands or
body systems
Endocrine System
Hormone
A substance that is released in one tissue
and travels through the circulation (usually) to
the target tissue.
Hormones reach all parts of the body, but only
target cells are equipped to respond
Hormones are secreted in small amounts and
often in bursts (pulsatile secretion)
Endocrine Functions
• Maintain Internal Homeostasis
• Support Cell Growth
• Coordinate Development
• Coordinate Reproduction , fertility, sexual
function
• Facilitate Responses to External Stimuli
4 Classes of Hormones
1.
Peptide/ Protein
(Range from 3 amino
acids to hundreds of amino acids in size. )
Steroid
3. Amine (Thyroid hormones
2.
and
Catecholamines)
4.
Eicosanoid
(Fatty acid derivatives )
The hormones fall into two general classes based
on their solubility in water.
The water soluble { amine (epinephrine) and
peptide/protein hormones} are secreted by
exocytosis, travel freely in the bloodstream,
and bind to cell-surface receptors.
The lipid soluble hormones { thyroid hormone,
steroid hormones and Vitamin D3}. diffuse
across cell membranes, travel in the
bloodstream bound to transport proteins, and
diffuse through the membrane of target cells .
Fat-soluble
hormone
Watersoluble
hormone
Signal receptor
Transport
protein
TARGET
CELL
(a)
Signal
receptor
NUCLEUS
(b)
Location of receptors
-
On cell surface
Peptides and proteins
In cytoplasm
Steroids
In nucleus
Thyroid hormones
Mechanisms of endocrine disease
Endocrine disorders result from:
Hormone deficiency,
(HRT)
Hormone excess
(Specific antagonists or release inhibitors )
Hormone resistance
(sensitizers)
Sources of hormones:
Natural
Human (GH; LH & FSH; hCG);
Animal (Insulin, T3 & T4)
- Biosynthetic
Insulin (Porcine & Bovine)
- Synthetic
Most hormones and their antagonists
-
DNA recombinant technology
Hypothalamic &
Pituitary Hormones
Cerebrum
Pineal
gland
Thalamus
Cerebellum
Pituitary
gland
Hypothalamus
Spinal cord
Hypothalamus
Posterior
pituitary
Anterior
pituitary
Hypothalamus and Pituitary
The output of the hypothalamus-pituitary unit regulates the
function of the thyroid, adrenal and reproductive glands and
also controls somatic growth, lactation, milk secretion and
water metabolism.
Hypothalamic Hs can have effect of stimulating or
inhibiting the release of ant. Pit. Hs. Called RELEASING
HORMONES “RH” or INHIBITING HORMONES “IH” respectively,
reflecting their influence on ant. Pit. Hs.
The Pituitary Gland
The Pituitary Gland is divided into 2 areas, with separate types
of hormone production.
The anterior pituitary makes and releases H under
regulation of the hypothalamus
Growth Hormone (GH)
Thyroid-stimulating Hormone (TSH)
Adrenocorticotropin (ACTH)
Follicle-stimulating Hormone (FSH) ),
Leutinizing Hormone (LH),
Prolactin
– The posterior pituitary stores and secretes H that are
made in the hypothalamus: oxytocin and antidiuretic
hormone (ADH)
Hypothalumus
Ant. pituitary
Growth hormone-releasing
hormone(GHRH) +
Growth hormone-releasing
inhibiting hormone
(GHRIH)_
Somatostatin
Growth Hormone (GH),
Thyrotropin-releasing
hormone (TRH)+
Thyroid Stimulating
Hormone (TSH),
Corticotropin-releasing
hormone (CRH)+
Adrenocorticotropic
Hormone (ACTH),
Gonadotropin-releasing
hormone (GnRH)+
Follicle-stimulating
Hormone (FSH),
Luteinizing Hormone(LH).
Dopamine _
Prolactin,
Post. Pituitary
Antidiuretic Hormone
Oxytocin
Hypothalamic hormones:
1- Growth Hormone- Releasing Hormone(GHRH):
Together with somatostatin controls release of the GH from
the ant. pit.
It is released from hypothalamus in a pulsatile
fashion, with 5-9 major pulses detected per day.
• GHRH release is enhanced by α2-adrenergic agonists
(e.g. clonidine) and opioids.
• GHRH release is increased by vigorous exercise.
Diagnostic Uses of GHRH (Sermorelin)
To test pituitary function in patients with GH deficiency.
GH deficiency could reflect either a hypothalamic or a pit. defect.
If the primary defect is hypothalamic, as is most common,
GHRH will elicit an increase in GH release.
If the defect is at the level of the pituitary, there will be no
increase in GH following GHRH administration.
Therapeutic Uses of GHRH to enhance GH secretion
Pulsatile subcutaneous delivery of GHRH, mimicking
the normal endogenous patterns (e.g. ~ every 3
hours) has been used to stimulate GH release in
patients with GH deficiency that is not of pituitary
origin.
IV, SC, intranasal
2- Somatostatin (Growth hormone-releasing
inhibiting hormone (GHRIH):
Inhibits GH release and TSH from the ant. pituitary .
Inhibits release of most GI hormones, reduces gastric acids and pancreatic
secretion. (glucagon , insulin & gastrin),
Therapeutic Uses Somatostatin
Somatostatin is of no clinical value because of it's short half-life (<3 min)
Octreotide ,a synthetic somatostatin analogue with a longer duration of action
Lanreotide is much longer acting, and is administered only twice a month.
used to treat: Acromegaly, Gastrinoma ,Glucagonoma & Other Endocrine
Tumors , and esophageal varices bleeding. (Inhibits Mesenteric vasodilatation induced by
glucagon)
A/E: GI disturb. postprandial hyperglycemia.
Gall stones often form as a result of decreased biliary flow and gall bladder
contraction.
3- Thyrotropin-Releasing Hormone(TRH):
Stimulates release of thyrotropin (TSH) from the ant pit.
Is used in diagnostic testing of thyroid dysfunction
Protirelin: IV
4- Corticotropin Releasing Hormone(CRH)
It stimulates secretion of both ACTH & beta –endorphin (a
closely related peptide ) from the ant. pituitary .
CRH can be used in the diagnoses of abnormalities of ACTH
secretion .
5- Gonadotropin-Releasing Hormone:(GnRH):
Stimulate the gonadotroph cell to produce and release LH
and FSH,
Gonadorelin, Buserelin, Nafarelin
GnRH agonists, SC infusion in pulses mimic physiological
GnRH, stimulates ovulation.
In contrast, steady dosing inhibits gonadotropin release by
causing down –regulation (desensitization) of GnRH
receptors in pituitary cells that normally release
gonadotropins .
GnRH is used in the diagnosis & treatment (by pulsatile
administration) of hypogonadal states in females & males .
Continuous GnRH agonists are used in sex H-dependent
conditions: prostate & breast cancers, uterine fibroids,
endometriosis or precocious puberty .
6- Prolactin-Inhibiting Hormone (PIH,dopamine):
Dopamine is the physiologic inhibitor of prolactin release
Because of its peripheral effects & the need for parenteral
administration, dopamine is not useful in the control of
hyperprolactinemia, but bromocrptine & other orally active
ergot –derivatives (eg. Cabergoline, pergoline) are effective
in reducing prolactin secretion from the normal glands as
well as from prolactinomas .
Also used in treatment of acromegaly
A/E: orthostatic hypotension, Psychiatric manifestations
Pituitary Hormones
Anterior pituitary
Hormones
Growth Hormone
•
Derived from the somatotroph cells
•
Its secretion is controlled by GHRH and somatostatin;
•
GH secretion is high in newborn, deceasing at 4 yr to an
intermediate level, which is then maintained until puberty,
when there is further decline.
•
Insulin-like growth factor 1 (IGF-1) released from the liver
inhibits GH secretion by stimulating somatostatin secretion
from the hypothalamus,
Growth Hormone Activity
1. Increases plasma free fatty acids (source of energy for
muscle tissue)
2. Increases hepatic glucose output
3. Decreases insulin sensitivity in muscle
4. Is protein anabolic hormone
Growth Hormone Deficiency
Can have a genetic basis or can be acquired as a result of
damage to the pituitary or hypothalamus by a tumor,
infection, surgery, or radiation therapy.
In childhood: short stature and adiposity, hypoglycemia.
Adults : generalized obesity, reduced muscle mass.
GROWTH HORMONE EXCESS
Mainly benign pituitary tumor
In adults causes acromegaly,
If this occurred before the long bone epiphyses
close, it leads to the rare condition, gigantism.
Treatment of excess GH disorders:
- Synthetic Somatostatin (Octreotide)
- DA agonists (Bromocriptine)
- Surgical removal / Radiotherapy of the tumor
- GH Antagonists (Pegvisomant)
An excess of GH can
cause gigantism,
while a lack of GH
can cause dwarfism
Clinical uses of GH
Somatotropin
GH deficiency in children & adults.
Children with short stature that is due to factors
other than GH deficiency:
Idiopathic short stature, Turner syndrome, Chronic renal
failure
A/E:
Hypothyroidism, Pancreatitis, Gynecomastia,
Possibilities of abuse have also arisen, e.g. creation
of “super” sports people.
Thyroid-stimulating Hormone (TSH)
Also called thyrotrophin
Stimulates secretion of thyroid hormone &
growth of thyroid gland.
Diagnostic Uses of TSH
In patients who have been treated
surgically for thyroid carcinoma, to test for
recurrence
Adrenocorticotropin (ACTH)
Stimulates cortisol secretion by the adrenal cortex &
promotes growth of adrenal cortex
Diagnostic use: as a test of the capacity of the
adrenal cortex to produce cortisol;
Follicle –stimulating hormone (FSH)
•
Females: stimulates growth & development of ovarian
follicles, promotes secretion of estrogen by ovaries.
•
Males: required for sperm production
3 preparations are available for clinical use:
Urofollitropin ,purified from of the urine of post menopausal
women,
2 recombinant forms, follitropin alpha & follitropin beta.
These products are used in combination with other drugs to
treat infertility in women & men.
Leutinizing hormone (LH)
•
•
Females: responsible for ovulation, formation of corpus luteum
in the ovary, and regulation of ovarian secretion of female sex
hormones.
Males: stimulates cell in the testes to secrete testosterone
• Lutropin alfa, approved for use in combination with
follitropin alfa for stimulation of follicular development in
infertile women with profound LH deficiency.
Prolactin
Secreted by lactotroph cells of the ant. Pit., which increase
in number during pregnancy.
Its secretion is stimulated by estrogen
•
Females: stimulates breast development and milk
production.
•
Males: involved in testicular function
No preparation of prolactin is available for use in prolactindeficient patients.
For patients with symptomatic hyperprolactinemia,
inhibition of prolactin secretion can be achieved with
dopamine agonists, which act in the pituitary to inhibit
prolactin release.
Posterior pituitary
Hormones
Oxytocin
•
It is synthesized in the hypothalamus & transported to
the post. Pit.
•
It is an effective stimulant of uterine contractions & is
used intravenously to induce or reinforce labor .
•
Induces the release of milk
•
Suckling sends a message to the hypothalamus via the
nervous system to release oxytocin, which further
stimulates the milk glands
Clinical uses of oxyticin
IV, IM
Induction of labor
Control of postpartum bleeding
A/E :
fetal distress, placental abruption, or uterine
rupture
excessive fluid retention
Vasopressin (antidiuretic hormone ADH)
•
It is synthesized in the hypothalamus & transported to the post.
Pit.
The function of ADH is to increase water conservation by the
kidney.
If there is a high level of ADH secretion, the kidneys reabsorb
water.
If there is a low level of ADH secretion, the kidneys release
water in dilute urine.
ADH release increases if blood pressure falls or blood becomes
too salty.
ADH causes peripheral blood vessel constriction to help elevate
blood pressure .
Clinical uses
Diabetes insipidus,
Nocturnal enuresis (by decreasing
nocturnal urine production)
A/E: hyponatremia and seizures
Synthetic ADH drugs
– Vasopressin: IV, IM
– Desmopressin: IV, IM. PO, intranasal