Introduction
This tutorial is designed to aid your learning of the endocrine system and also as a useful revision tool. It
should be an addition to your further reading, and not the only learning you do on this topic.
It should take you approximately 40 minutes to complete.
To navigate through the tutorial, use the arrows in the top or bottom right corners or the contents column
on the left. There are questions throughout the tutorial for you to check your learning as you go.
Objectives
1. To help you revise the anatomy and embryology of the hypothalamus and pituitary glands.
2. To cover the hormones released from theses glands and their action on other glands or organs in the
body.
3. To use case studies and interactive questions to consolidate clinical learning of the different conditions
associated with these glands.
Embryology and Anatomy
The hypothalamus and pituitary glands are both very closely related in terms of position and function. The
following pages should be revision for you.
Embryology
Embryologically, the hypothalamus is part of the forebrain.
The pituitary is divided into two sections - the anterior pituitary and the posterior pituitary. These develop
separately in the embryo.
The anterior pituitary comes from the ectoderm of the primitive mouth (Rathke's Pouch). It moves
upwards to join the infundibulum from the hypothalamus. When its original blood supply is lost travels, it
develops a new one from the hypothalamus. This blood supply is the only communication between the
hypothalamus and the anterior pituitary.
Because the anterior pituitary moves upwards during development, there is a possibility of small clusters of
epithelial cells being left behind along the path and these may develop into cysts or ectopic hormonesecreting tumours later in life.
The posterior pituitary develops from neuroectoderm and grows down from the hypothalamus. This allows
neurosecretory cells to join the hypothalamus and the posterior pituitary, forming their only means of
communication.
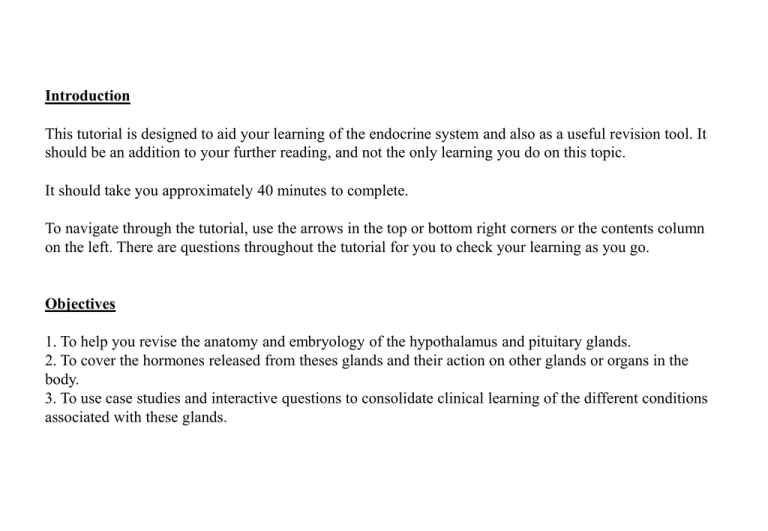
Anatomy
The hypothalamus lies underneath the thalamus, at the base of the forebrain. It is a link between the
neurological and endocrine systems.
The pituitary gland is made up of two parts, the anterior and posterior pituitary. It sits in an indentation into
the sphenoid bone called the sella tursica, covered over by the diaphragma sellae which is a thin piece of
fibrous tissue.
The pituitary gland lies directly beneath the optic chiasm which means that any large tumours of the
pituitary can press on the chiasm and cause visual disturbances (an important symptom to remember!)
The pituitary stalk (infundibulum) connects the posterior pituitary to the median eminence of the
hypothalamus.
The anterior pituitary is divided into 3 parts:
1. Pars distalis (the main part of the gland)
2. Pars intermedia (this lies between the anterior and posterior parts of the gland and consists of
corticotroph cells)
3. Pars tuberalis (this surrounds the infundibulum and contains mostly gonadotroph cells)
The blood supply to the hypothalamus is from the superior hypophyseal artery. The blood then travels via
portal veins, through the median eminence, to the anterior pituitary. It drains to the cavernous sinuses.
The blood supply to the posterior pituitary is from the inferior hypophyseal arteries and it also drains to
the cavernous sinus.
Connections between the Hypothalamus and Pituitary
The anterior pituitary is made up of secretory epithelial tissue and is attached to the hypothalamus by
a portal venous blood supply. The hypothalamus releases hormones into these veins and they then
stimulate or inhibit the pituitary tissue. When cells of the anterior pituitary are stimulated, they release
their hormones into the systemic circulation.
The posterior pituitary is made of neuroendocrine tissue, so although it also derives a blood supply
from the hypothalamus, this is not how it receives its instructions. Instead, neurosecretory cells run
from the hypothalamus down to the posterior pituitary. The axon terminals are located next to blood
sinusoids and release neurosecretory granules when the cells are stimulated. The cells of the posterior
pituitary itself are glial cells that support the axons of cells that originate in the hypothalamus.
Negative Feedback
The endocrine system works on the basis of negative feedback. You should be comfortable understanding
and reproducing diagrams like these.
Hormones of the Hypothalamus
Hormone
Cells affected in the anterior
pituitary
Effect
Growth hormone releasing
hormone (GHRH)
Somatotrophs
Increased GH release
Growth hormone inhibiting
hormone (GHIH/somatostatin)
Somatotrophs and thryotrophs
Decreased GH and TSH release
Corticotrophin releasing hormone
(CRH)
Corticotrophs
Increased ACTH release
Gonadotrophin releasing hormone
(GRH)
Gonadotrophs
Increased LH and FSH release
Thyrotrophin releasing hormone
(TRH)
Thyrotrophs and lactotrophs
Increased TSH and prolactin release
Prolactin releasing factors
(PRF)
Lactotrophs
Increased prolactin release
Dopamine
(prolactin inhibiting hormone)
Lactotrophs
Decreased prolactin release
Hormones of the Anterior Pituitary
Hormone
Effect
Stimulated
By
Supressed by
Produced By
Growth Hormone
(GH)
Stimulates the liver to produce IGF-1
opposes the action of insulin
GHRH
GHIH and IGF-1
Somatotrophs
Thyroid Stimulating
Hormone (TSH)
Stimulates the thyroid gland to release
thyroxine
TRH
T3
Thyrotrophs
Adrenocorticotrophic
Hormone (ACTH)
Stimulates the adrenal cortex to release
glucocorticoids and androgens
CRH
Glucocorticoids
Corticotrophs
Luteinising Hormone
(LH) and Follicle
Stimulating Hormone
(FSH)
Causes the release of sex steroids from
reproductive organs
GnRH and
sex steroids
Prolactin and sex
steroids
Gonadotrophs
Prolactin
Initiates lactation and promotes growth
of mammary glands and reproductive
organs
PRF and TRH
Dopamine
Lactotrophs
MelanocyteStimulating Hormone
(MSH)
Stimulates melanin synthesis in
melanocytes in the skin
–
–
Corticotrophs
Beta-Endorphin
Not yet fully understood, but possibly
involved in pain control
–
–
Corticotrophs
The first 6 hormones in the table are the main hormones from the anterior pituitary, so you should
make sure you know these for your exams.
This mnemonic might help:
Those Pituitaries Are Fun Little Glands
Hormones of the Posterior Pituitary
Hormone
Effect
Produced By
Stimulated By
Suppressed
By
Anti-diuretic
Hormone
(ADH)
Increases the permeability of the
collecting ducts in the kidneys, causing
greater reabsorption of water
Supraoptic
vasopressinergic
neurons
Raised
osmolarity, low
blood volume
Reduced
osmolarity
Oxytocin
Causes smooth muscle contraction of the
uterus (leading to birth) or the mammary
glands (leading to milk ejection)
Paraventricular
oxytocinergic
neurons
Stretch
receptors in the
nipple or cervix,
oestrogen
Stress
Remember that anti-diuretic hormone (ADH) is also known as vasopressin, or sometimes as arginine
vasopressin (AVP)
Disorders of the Hypothalamus and Pituitary
Presentation
Disorders relating to these two glands usually present with symptoms of a deficiency or excess of
one or more of the hormones that they produce. So, if you know the hormones, where they come
from and what effect they have, you should know enough to work out most diagnoses.
The other symptoms that patients could present with are neurological, such as headaches and visual
disturbances from tumours of these glands affecting surrounding structures.
The first stage of working out a diagnosis is to work out which hormones are affected and whether
there is an excess or a deficit. The next stage is to work out why the hormone has been affected. As
with many conditions, you should think about a list of possibilities.
5 Main Causes
Idiopathic
Invasion (i.e. tumours)
Infarction (e.g. Sheehan's syndrome)
Iatrogenic (surgery, radiotherapy or certain drugs)
Injury (i.e. head trauma)
Very Rare Causes
Infection (e.g. tuberculosis)
Infiltration (e.g. sarcoidosis)
Inherited (e.g. congenital hormone deficiency)
Immunological (e.g. lymphocytic hypophysitis)
You should certainly be aware of the 5 main causes in order to come up with a reasonable differential
diagnosis.
Investigations
There are 3 types of investigations that can be done in these cases:
1. Basal Blood Tests
2. Dynamic Tests
3. Imaging
Hormones that are relatively constant in the blood, such as TSH, can be measured as a baseline test.
This means the blood test can be taken at any time because the results of a healthy individual should
always lie in a particular range. Other hormones that fluctuate (e.g. FSH and LH levels vary over a
month, GH and ACTH vary over a day and also with stress) can be measured in this way as well, but
consideration must be made for the time and situation when they were taken.
In cases where basal test results are unclear, it is better to perform dynamic tests. Dynamic tests are
either suppression or stimulation tests. If a hormone is stimulated, but levels do not rise, then there
must be a problem with the production of that hormone. If an inhibiting substance is given, but
normal negative feedback does not occur, then there is likely to be a hormone-producing tumour
causing the symptoms.
If a tumour is suspected, imaging is used to determine the location of the tumour and its suitability
for surgical treatment. This is usually MRI imaging (on MRI, a micro adenoma is classified as more
than 10mm, and a macro adenoma is less than 10mm).
Treatment
There are 3 main forms of treatment:
1. Replacement hormones
For deficiency problems or when other treatments designed to reduce excess hormone output
destroy too much glandular tissue
2. Surgery or radiotherapy
For tumours
3. Drugs that inhibit hormone production
When surgery or radiotherapy is not suitable
Acromegaly
Acromegaly is caused by hypersecretion of GH, usually due to a pituitary tumour.
In children, the condition is called gigantism.
It is a rare condition (prevalence = 5 per million).
The age of onset is usually between 30 and 50.
The most common cause of GH hypersecretion is a functioning somatotroph ademona.
The symptoms and signs in an adult are mostly caused by the growth of soft tissues and some bones.
Clinical Symptoms
Clinical Signs
Enlarged hands and feet
Enlarged skull circumference
Enlarged liver, kidneys and heart (predisposes to
cardiomyopathy)
Coarse, thickened skin (leads to prominent
nasolabial folds and supraorbital ridge)
Large lower jaw, nose and tongue
Spacing between the lower teeth
Greasy sweating and Temperature intolerance
Mental disturbance and insomnia
Loss of peripheral vision (compression of the optic
chiasm by a tumour)
Carpal Tunnel Syndrome
1 in 3 have hypertension (predisposes to ischaemic
heart disease)
1 in 10 are hypercalcaemic
1 in 4 are glucose intolerance (increases risk of
developing diabetes)
Altered bone structure (predisposes to osteoarthritis)
1 in 5 have hyperthyroidism
In children, the GH causes an increase in the growth of long bones. This results in the child being tall
for their age. They may be of an average height when they reach adulthood because GH also causes the
epiphyses to fuse at an earlier age. The main problem with gigantism is the risk of diabetes.
The oral glucose tolerance test is the investigation of choice in making the diagnosis of acromegaly:
Glucose and GH are measured at 30 minute intervals for 150 minutes. Insulin is released in response to
the glucose. In healthy people, insulin causes suppression of GH. However, if there is no suppression or
if levels of GH rise, this is diagnostic of acromegaly.
Adenomas are surgically removed if possible. If not, external radiation or medical treatment are options.
The drugs that can be used are somatostatin (GHIH) analogues – ocreotide or lanreotide.
Follow ups are very important to monitor:
1. Growth Hormone Levels
2. Glucose Tolerance
3. Cardiovascular System Function
4. Thyroid Hormone Levels
5. Prolactin Hormone Levels
6. Visual fields
Cushing’s Syndrome and Cushing’s Disease
Cushing's syndrome describes a chronic excess of glucocorticoids .This may be due to hypersecretion
from the anterior pituitary or adrenal glands, excess steroid medication or ectopic ACTH production.
Clinical Symptoms
Clinical Signs
Truncal obesity
Supraclavicular fat pad
Purple abdominal striae
Thin hair/male pattern baldness
Depression, confusion, psychosis, insomnia
Round “moon” face (due to facial fat deposition)
Acne
Hirsutism (coarse pigmented hair growth on the face,
chest or abdomen)
Thin, easily bruised skin
Wasting/weakness of skeletal muscle (leads to thin
arms and legs)
Menstrual cycle disturbances
Renal calculi
Predisposition to infection (also means wounds heal
more slowly)
Hypertension
Predisposition to congestive cardiac failure
Osteoporosis, vertebral collapse
Predisposition to glucose intolerance/diabetes
Cushing's disease specifically describes an adenoma of corticotrophic cells of the anterior pituitary. The
symptoms are the same as for Cushing's syndrome, except the patient also has pigmented skin because
the cells that make excess ACTH also make excess MSH.
The investigations of excess glucocorticoid:
A 24 hour urinary free cortisol test is often performed to determine that the patient’s symptoms are
because of increased cortisol levels. Doing the test over 24 hours means that circadian rhythm does not
affect the interpretation of the results. Normal levels of cortisol in the urine should be less than
280nmol/24hr.
The other screening test used is the Overnight Dexamethasone Suppression Test;
Plasma cortisol is measured, and then 1mg of oral dexamethasone (a synthetic glucocorticoid) is given
at midnight. The plasma cortisol is measured again at 8am. This would suppress cortisol levels to less
than 50nmol/L in a healthy subject. In patients with excess cortisol, levels will not be suppressed or
suppressed very little.
Once you have determined that the patient has excess cortisol, you need to work out where the problem
is. There are three main possibilities when thinking about a patient with Cushing’s syndrome.
1. Pituitary adenoma (Cushing’s Disease) producing excess ACTH
2. Ectopic ACTH production from a tumour (often small cell lung cancer or carcinoid tumour)
3. Adrenal adenoma or carcinoma producing excess cortisol
The first test necessary to distinguish between these causes is a plasma ACTH test;
Plasma ACTH – if the problem is with hypersecretion from the adrenal glands, the ACTH levels will be
suppressed to undetectable amounts (because of negative feedback).
If the ACTH is normal or high, you need to distinguish between pituitary and ectopic ACTH. The first
line test is a high-dose dexamethasone suppression test;
High-dose dexamethasone suppression test (2mg, 6 hourly for 48 hours) – if the patient has Cushing’s
disease, this will cause at least partial depression of cortisol levels. This is because the exogenous
cortisol will still have some negative feedback effect if the problem is pituitary-based. If there is no
suppression at all at high levels, then the source must be ectopic, such as a small cell lung cancer
because these will not have feedback receptors.
Having done these tests to determine the cause of excess cortisol or ACTH, imaging may be required
to further investigate the adrenals or pituitary, or to look for a hormone-producing tumour.
These diseases have a mortality rate of 50% at 5 years, so effective treatment is very important.
Treatment options:
1. Pituitary adenomas can be treated with surgery.
2. Iatrogenic causes are treated by removing the source if possible.
3. Drug therapy using agents such as metyropone or aminoglutethimide to reduce levels of cortisol in
the plasma.
4. Adrenal adenomas/carcinomas are treated with surgical resection, after preparatory treatment with
metyropone to reduce the risks of surgery.
Medical therapy is also used as palliative treatment in cases where a malignancy is not resectable.
Hyperprolactinaemia
Hyperprolactinaemia is the most common hormone dysfunction of the pituitary. 50% of pituitary adenomas
are prolactinomas.
Other causes of increased prolactin secretion are disinhibition by reducing local dopamine levels (e.g. from
pituitary stalk compression) or by administration of a dopamine antagonist.
Clinical Symptoms
Clinical Signs
Female
Decreased libido
Weight gain
Amenorrhoea (cessation of menstrual cycle)
Galactorrhoea (inappropriate production of
breast milk)
Infertility
Osteoporosis
Neurological signs (from pressure of pituitary
tumour)
Male
Reduced facial hair
Impotence
Galactorrhoea
Osteoporosis
Neurological signs (from pressure of pituitary
tumour)
The investigations for hyperprolactinaemia are very simple:
A basal test is done between 9am and 4pm. If the levels are significantly raised, the pituitary fossa will be
imaged, since the higher the level of prolactin, the more likely it is that the problem is a functioning adenoma.
Treatment is surgery if possible, but radiotherapy or drug treatment if not. The dopamine agonists given may
be teratogenic so should not be given to a pregnant woman or a woman who is trying to get pregnant.
Hypopituitarism
Hypopituitarism has several causes:
1. Non-functioning pituitary adenomas
2. Other tumours in surrounding tissues compressing the pituitary gland
3. Infarction of the pituitary gland -e.g. Sheehan's Syndrome
4. Compression of the pituitary gland -i.e. Empty Sella Syndrome
5. Trauma
6. Hypophysectomy (surgical removal of the pituitary) or radiotherapy
Sheehan’s Syndrome
Infarction of the pituitary gland occurs if there is a large amount of blood loss during labour. The drop in
blood pressure leads to infarction of the pituitary which is very sensitive to hypoxia in pregnancy.
Empty Sella Syndrome
A condition in which cerebrospinal fluid gets into the sella turcica and compresses the pituitary gland.
Approximately 50% of people have this condition without it becoming pathological. It may be due to a
congenital defect in the diaphragma sella, pituitary surgery or radiation, pituitary infarction or a pituitary
tumour.
Deficient Hormone
Clinical Symptoms
Clinical Signs
Corticotrophin
Dizziness
Nausea
Postural hypotension
Breast atrophy
Weight loss
Hyponatraemia
Gonadotrophin
Oligomenorrhoea/amenorrhoea
Decreased libido
Infertility
Osteoporosis
Androgen
Hair loss
Decreased libido
Erectile dysfunction
Hypogonadism
Growth Hormone
Truncal obesity
Weakness
Atherosclerosis
Decreased cardiac output
Osteoporosis
Thyroid Hormones
Weight gain
Dry skin
Constipation
Low mood
Investigations
Basal level tests are done for the following hormones:
Prolactin
TSH (and TSH)
LH
FSH
The following hormones are tested with dynamic tests:
GH (insulin tolerance test)
ACTH (insulin tolerance test or short synacthen test)
Insulin Tolerance Test:
Insulin is giving intravenously to induce hypoglycaemia. GH (and cortisol) should rise in a normal
person.
Short Synacthen Test:
Synacthen is an ACTH analogue and as such, should induce a rise in cortisol levels in a healthy
individual.
Treatment
The treatment is to remove any tumour if possible. If not, then the pituitary hormones must be replaced.
Hormone
Replaced With
GH
Subcutaneous replacement with human recombinant GH
ACTH
Oral cortisol replacement
TSH
Oral thyroxine
Oestrogen and
Progesterone/Testosterone
Oral oestrogen and progesterone is given cyclically to females, oral or
intramuscular testosterone is given to males
LH and FSH
If male or female fertility is required, intramuscular human chorionic
gonadotrophin, LH and FSH are given
This is a lifelong treatment.
Diabetes Insipidus
There are 2 types of diabetes insipidus;
1. Cranial DI (ADH release from the pituitary is deficient)
2. Nephrogenic DI (ADH receptors in the kidney do not function properly)
Both result in the following symptoms:
Clinical Symptoms
Polyuria
Dilute urine
Polydipsia
Dehydration (if not drinking
sufficient water)
Causes of Cranial DI
Causes of Nephrogenic DI
Head Injury
Hypophysectomy
Metastases
Pituitary Tumour
Meningitis
Vascular Lesion
Sarcoidosis
Inherited
Idiopathic (usually self-limiting)
Low Potassium
High Calcium
Drugs (e.g. lithium)
Pyelonephritis
Hydronephritis
Inherited
Pregnancy (rare as a primary
cause)
Investigations
The first investigation needed is to determine whether there is a problem with ADH. This is done using a
Water Deprivation Test;
The patient is deprived of food and water for a night and then for 8 hours the following day. Plasma and
urine osmolality is monitored regularly. The patient's weight is also monitored (and the test is abandoned
if more than 3% body weight is lost). If the urine osmolality remains low then the patient can be
diagnosed with diabetes insipidus (this shows that the body cannot concentrate the urine in response to
dehydration).
The second part of the test is to find out whether the problem is a lack of ADH (cranial DI) or
insensitivity of the ADH receptors in the kidneys (nephrogenic DI). This is a suppression test called the
Desmopressin Test;
This is done immediately after the water deprivation test so that the patient is still fasted and dehydrated.
Desmopressin, an ADH analogue is given and the patient is given water to drink. The urine and plasma
osmolality is measured 2 hours later. If the problem was cranial DI, then giving an analogue should return
the osmolalities to normal. If it is a nephrogenic DI then the desmopressin will have no effect.
Treatment
The treatment for cranial diabetes insipidus is life-long treatment with desmopressin which is a long-acting
ADH analogue. This is given intranasally.
An excess of ADH is called syndrome of inappropriate ADH secretion (SIADH). This is an important
cause of hyponatraemia.
Clinical Symptoms
Clinical Signs
Confusion
Symptoms
Nausea
Muscle Weakness
Hypertension
Cardiac Failure
Low Serum Sodium
SIADH can be distinguished from other causes of hyponatraemia by the 4 following features:
1. The patient is not dehydrated/no hypovolaemia
2. No oedema
3. Concentrated urine
4. No diuretic use
Treatment is by treating the cause and restricting fluids.
Conclusion
The important points to take away from this tutorial:
1. Know what negative feedback is and be able to describe it.
2. Know the hormones released from the hypothalamus and pituitary.
3. Understand the roles of these hormones.
4. Know about the major diseases caused by deficiency and excess of these hormones.