HF-Taumarunui
advertisement

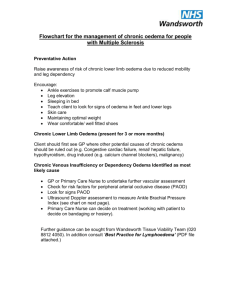
The Waikato Integrated Heart Failure Service (WIHFS) Debbie Chappell CNS Heart Failure Taumarunui/Te Kuiti/Otorohanga/Te Awamutu The Waikato Integrated Heart Failure Service Team HF CNSs: • Julie Jay, Eileen Gibbons, Karyn Haeata,Debbie Chappell, Simona Inkrot, Catherine Callagher Cardiologists: • Mark Davis, Gerry Devlin, Raewyn Fisher Sonographers HF in Aotearoa/NZ 2 % Heart Failure prevalence in Western societies HF Incidence is rising with an ageing population and the improved treatment and survival of heart disease Median survival of 3.5 years after initial HF admission in NZ One-year HF mortality rates after initial hospital admission are between 25 and 35% Maori patients admitted with HF are significantly younger than NZ European: mean age 62 vs. 78 years McMurray et al., 2012; Wasywich et al, 2010; Schaufelberger et al., 2004; Wall et al., 2012 Refresher A&P Definition Heart Failure is a clinical syndrome where the heart is unable to pump blood at a rate required by the body, patients present with some or all of the following features: Symptoms typical of heart failure (breathlessness at rest or on exercise, fatigue, tiredness, ankle swelling) AND Signs typical of heart failure (tachycardia, tachypnoea, pulmonary rales, pleural effusion, raised jugular venous pressure, peripheral oedema, hepatomegaly) AND Objective evidence of structural or functional abnormality of the heart at rest (cardiomegaly, third heart sound, cardiac murmurs, abnormality on the echocardiogram, raised natriuetic peptide concentration) Normal HF-REF HF-PEF Some causes of heart failure • • • • • • • • • Coronary artery disease Hypertension Valvular heart disease Cardiomyopathies Endocrine disorders-thyrotoxicosis Genetic conditions Congenital heart disease Inflammatory Chronic arrhythmias • Also think of co morbidities – diabetes, obesity, COPD Pathophysiology Compensatory mechanisms of acute heart failure • Sympathetic nervous system activation • Renin-angiotensin system activation • LV remodelling OUTCOME: • Vasoconstriction – Increased HR, SV leads to increased CO • Attempt to maintain cardiac output and vital organ perfusion – heart, brain, kidneys Maladaptation • Compensatory mechanisms become “maladaptive” in chronic heart failure OUTCOME: - Excessive vasoconstriction - Increased afterload - Excessive salt and water retention - Electrolyte abnormalities - Arrhythmias Investigations • Observations – TPR BP (lying/standing), weight, height BMI • ECG – old and new changes • Bloods – CBC, U&E, Cardiac enzymes, NT-pro BNP, LFT, Cholesterol, TFT • CXRay – old and new • ECHO- normal EF >55%, moderate – severe HF<40% Treatment Options – medical vs intervention Pharmacological - Diuretics -ACEi -Beta-blockers -Other drugs Non pharmacological -fluid management -nutrition -physical activity -smoking -psychosocial support -other factors Case studies • 75 year old female • History incr SOBOE (getting worse) • Bilateral pitting oedema • JVP +2, chest clear • • • • History hypertension Dip stick, LFT, U&E NT pro BNP 400 pg/mL Refer - ECHO normal LV, elevated filling pressures, HFpEF • Treatment options • • • • 49 year old male Bilateral oedema, pants tight Appetite depressed JVP normal, ascites, ? pulsatile liver • Jaundiced • • • • • Dip stick (bilirubin) LFT - abnormal NT pro BNP – normal Renal – normal Check ? Hepatitis, alcohol, blood transfusion Aims of treatment / nursing role • Improve symptoms – fluid restrict, daily weigh, medication • Improve LV function – medication, medical intervention • Improve exercise tolerance – moving, pacing themselves • Improve patient education & self-management – HF booklet • Decrease hospital admissions - improve survival • End of life care CNS led interventions for HF patients Decreased hospitalisation, decreased number of events, readmissions and days in hospital Improved survival Cost effective Improved self-care behaviour Stromberg et al., 2003; Phillips et al., 2005 Referral Criteria Inclusion: • Patients with possible heart failure and/or at high risk for heart failure in the community, e.g. previous MI, family history of cardiomyopathy • Patients readmitted for heart failure within 3 months • Heart failure patients with significant co-morbidities affecting optimisation of treatment • “Shared care” for end stage/palliative care Exclusion: • Lack of consent from patient • Acute coronary syndrome • Patients already under the care of a cardiologist, unless referred by this cardiologist (inclusion criteria must be satisfied) COMPONENTS OF WIHFS • Specialist clinics (CNS and cardiologists), Home visits, Telephone care – Patient and family/whanau education: heart failure knowledge and self-care – Clinical monitoring – Titration of heart failure medications in consultation with GP and/or cardiologist • Professional education/CME for other health professionals and community teams Thank you Debbie Chappell – Taumarunui Te Kuiti/Otorohanga/Te Awamutu 0212419452 07 8785192 Questions?