Chronic Sinusitis
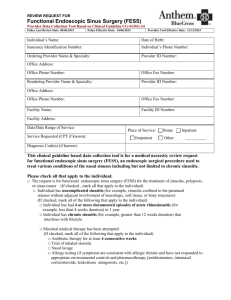
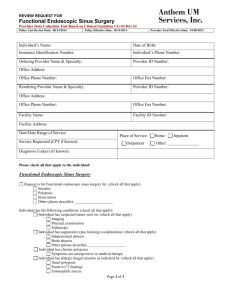
advertisement
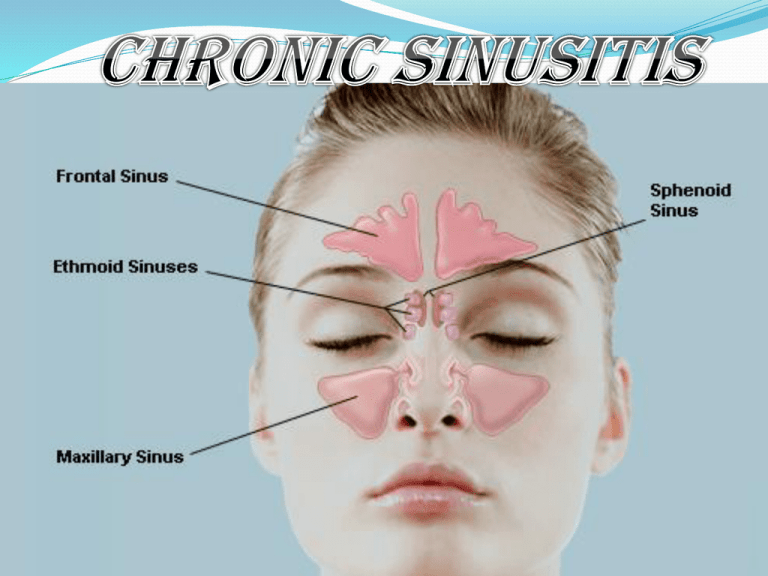
Definition Chronic inflammation of the mucosal lining of one or more paranasal sinuses, usually caused by anatomical / pathological obstruction to its drainage, and is characterized by chronic postnasal mucopurulent discharge with or without recurrent headache / facial pain. (more than 1month). Types Open / Close Unilateral / bilateral Single sinus / multi-sinusitis / pan-sinusitis Anterior group / posterior group Suppurative / Hypertrophic Osteomeatal complex : before and after fess Mucociliary function Etiopathogenesis Usually Rhinogenic. Other routes- rare. Unresolved acute sinusitis Any form of rhinitis Mucosal odema in OMC Pathological obstruction Any anatomical variation obstruction Anatomical Stagnation and secondary chronic sinusitis Infective / reactive rhinitis Mucosal odema/ polyp formation Pathological mucous/ mucociliary dysfunction Mechanical: DNS, anatomical variations in the MM/ OMC, etc. Anatomical obstruction Pathological obstruction Impaired drainage of sinuses in the MM/ OMC Stagnation and secondary infection Chronic sinusitis Pathogenesis : Mucosal odema Mechanical obstruction (anatomical) Mucous- thick Primary mucociliary dysfunction Anterior ethmoids is the key area for causation of chronic anterior group sinusitis because Ostiomeatal complex is situated within it Acts as reservoir of infection Types & Mucosal changes Open/ closed type Mucosal changes: Hyperemia Hypertrophy Increased mucosal glands Polypoidal changes Mucopurulent secretions Microabscesses Fibrosis, hyalinization Atrophy, squamous metaplasia, granulations Bacteriology Mixed infection Streptococcus pneumoniae, Hemolyticus, Staph aureus, gram negative bacteriae,etc. Anaerobic infection> fowl smelling discharge Clinical features: Symptoms Mucopurulent/ purulent post nasal discharge Cachosmia- anaerobic Headache/ facial pain- depending on the site and type- usually dull aching. Nasal obstruction Aural and throat symptoms Clinical features: Signs Discharge in the MM on anterior rhinoscopy Mucosal changes in the MM Discharge in MM/ SM on posterior rhinoscopy Tenderness in acute excerbations Postural/ Transillumination tests Prominent lateral pharyngeal band Investigations Plain radiographs “Water’s” Mucosal thickening, haziness, opacity, polyp CT scan of OMC/ paranasal sinuses (coronal cuts) X-ray nasopharynx in children Diagnostic nasal endoscopy Allergic tests if suspected Proof puncture for maxillary sinus Culture and sensitivity- rarely done Fungal culture of cheesy discharge, if present CHRONIC Sinusitis Endoscopic appearance of mucosal changes in CHRONIC sinusitis Treatment: Medical Antibiotics Nasal decongestants- topical/ systemic Antihistaminics Analgesic-antiinflammatory Medicated steam inhalation Alkaline nasal douches Steroid nasal spray/ short course of systemic steroids Antiallergy treatment Treatment: Surgical When refractory to medical treatment Surgery for predisposing causes like DNS, polyp, etc. Surgical procedure depends on the sinus involved All sinuses may be surgically accessed endoscopically Chronic maxillary sinusitis Surgical options Antral puncture Intranasal antrostomy Caldwel-Luc operation FESS (Functional endoscopic sinus surgery) •Opening through canine fossa •Counter opening into inferior meatus •Radical mucosal debridement CALDWELL LUC SURGERY Chronic ethmoiditis Intranasal ethmoidectomy Blind & dangerous Trans-antral ethmoidectomy Via Caldwel-Luc operation External ethmoidectomy (Howarth operation) Endoscopic ethmoidectomy (FESS) Chronic frontal sinusitis External frontoethmoidectomy (Lynch-Howarth operation) Osteoplastic operation Obliteration of frontal sinus Endoscopic frontal sinusostomy Chronic sphenoidal sinusitis Intranasal sphenoethmoidectomy External sphenoethmoidectomy Endoscopic sphenoidotomy Functional endoscopic sinus surgery (FESS) Uncinectomy (infundibulotomy) Middle meatal antrostomy Frontal recess clearance Anterior ethmoidectomy