Otitis, Sinusitis and Bronchitis
advertisement

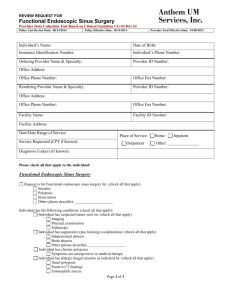
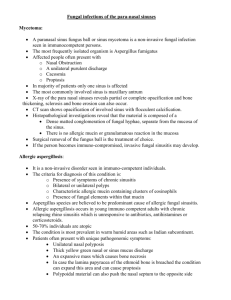
Michael De Vito M.D. Capital Region Otolaryngology Group Albany, Troy, Clifton Park and Hudson Introduction Sinusitis: Affects 30 million individuals per year in the US 90% of patients will see their primary care physician Accounts for 11.6 million visits to primary care physicians annually Accounts for 9% of pediatric and 21% of adult antibiotic prescriptions Anatomy Anatomy Sinus Drainage Pathways Pathogenesis of Sinusitis Classification of Sinusitis Sinusitis is defined as an inflammation of the mucous membrane that lines the paranasal sinuses It is classified chronologically as: Acute Recurrent Acute Subacute Chronic Acute Exacerbation of Chronic Acute Rhinosinusitis • A New Infection That May Last Up To Four Weeks • Can Be Subdivided Symptomatically Into Severe Non-severe Recurrent Acute Rhinosinusitis • Four or More Separate Episodes of Acute Sinusitis That Occur Within One Year Subacute Rhinosinusitis • An Infection That Lasts Between Four to Twelve Weeks • Usually Represents a Transition From Acute To Chronic Infection Chronic Rhinosinusitis • When Signs and Symptoms Last for More Than Twelve Weeks Diagnosis of Sinusitis Viral Versus Bacterial Rhinosinusitis • Viral Upper Respiratory Illnesses Occur: 3-8 per year in children 2-3 per year in adults • Gwaltney: (1996,1994) Found 90% of CT Scans Showed Evidence of Sinus Involvement With Viral Rhinosinusitis Viral Upper Respiratory Infection Course Viral Versus Bacterial Rhinosinusitis Difficult to Differentiate Symptoms of Bacterial Sinusitis Worsen After Five Days Bacterial Infections Persist For At Least Ten Days Task Force On Rhinosinusitis Of The AAO-HNS Diagnosis of Acute Sinusitis Depended On The Presence of : Two Major Diagnostic Factors or One Major Factor and Two Minor Factors Diagnostic Predictive Factors of Sinusitis Acute Sinusitis Definitions Radiographic Imaging • Radiographic Imaging Should Not Be Used In Patients That Meet The Diagnostic Criteria of Acute Rhinosinusitis • Exceptions Include: A Potential Complication of Sinusitis An Alternative Diagnosis is Suspected Symptomatic Treatment Analgesics and Antipyretics for Pain and Fever Topical or Systemic Decongestants for Symptomatic Relief Neither have been proven to prevent a URI from becoming ABRS Topical Better Than Systemic for Congestion Relief 3 Day Maximum – Longer Rebound Concern Systemic Steroids Have Shown No Effectiveness Antihistamines Have No Studies As To Effectiveness Symptomatic Treatment • Topical Steroid Sprays Have Shown Some Benefit Industry studies and included antibiotics • Nasal Saline for Quality of Life Improvement Decrease medication use for frequent ABRS • Guaifenesin Insufficient evidence • Most Prevalent Pathogens in Adult Sinusitis Staphylococcus aureus (0-8%) Other (4%) Moraxella catarrhalis (2-10%) Streptococcus pneumoniae (20-43%) Anaerobes (0-9%) Streptococcus spp. (3-9%) 1. 2. Sinus and Allergy Partnership. Otolaryngol Head Neck Surg 2004. AAOHNS. Otolaryngol Head Neck Surg. 2007. Haemophilus influenzae (22-35%) Empiric Treatment in Children Amoxocillin-clavulanate Rather Than Amoxocillin Increasing prevalence of H. influenza in URIs in children High prevalence of Beta-lactamase producing pathogens in ABRS H. influenza and Moraxella catarrhalis IDSA 2012 Clinical Practice Guidelines for Acute Rhinosinusitis Antibiotic Regimen in Children Starting Empiric Antibiotic Treatment • In Adults When Clinical Diagnosis Has Been Established By The Guidelines • Symptoms of rhinosinusits lasting more than 10 days • Severe symptoms or high fever and purulent nasal discharge or facial pain lasting 3-4 consecutive days at the onset of illness • Worsening of symptoms with fever, headache or increased nasal discharge at day 5-6 of a URI that were improving. IDSA 2012 Clinical Practice Guidelines for Acute Rhinosinusitis Antibiotic Regimen for Adults Treatment of Penicillin Allergic Patients • Skin Testing to Confirm of Exclude Immediate Hypersensitivity • Adults: Respiratory Floroquinolone (Levofloxacin,Moxifloxacin) Doxycycline Macrolides or TMP/SMX No Longer Recommended because of increased resistance of S. pneumonia and H. influenza Children with Penicillin Allergy • Children with Type 1 Hypersensitivity: Levofloxacin FDA approved for use only after Anthrax Exposure 2523 Children Studied in the Pediatric Levaquin Study (Noel, 2007) Well tolerated after 12 Months But Musculoskeletal Events 1.9% vs. .79% at 2 months 2.9% vs.1.6% at 12 months Probably Warranted with Type 1 sensitivity Children with Non-Type 1 • Third Generation Oral Cephalosporin: Cefixime, Cefpodoxime • In Combination With Clindamycin Duration of Therapy 5-7 Days Seems Appropriate Most patients studied by sinus puncture had symptomatic improvement and bacteriological eradication within 72 hours of initiation of treatment Treatment beyond 10 days for acute , uncomplicated patients seems excessive • Children Should Be Treated for 10-14 Days Studies still lacking to recommend less Nonresponsive Patients • Patients Who Clinically Worsen After 72 Hours or Fail to Improve After 3-5 Days of Empiric Therapy: Resistant Pathogens Noninfectious Etiology Structural Abnormalities • CT of MRI Noninfectious causes of suppurative complications • Sinus or Meatal Cultures • Careful Clinical Assessment Sinus Cultures Direct Sinus Aspiration : Most Accurate but Invasive , Not Well Tolerated Middle Meatal Cultures: Benninger (2006) 81% sensitivity, 91% specificity, 83% predictive value Nasopharyngeal Swabs: Unreliable Allergy Evaluation Chronic Sinusitis And Allergy: 40-80% of Adults 25-31% Young Adults Should Be Considered In: Chronic Rhinosinusitis Recurrent Acute Rhinosinusitis Skin Testing As The Preferred Testing Method Immunodeficiency Patients with Chronic Rhinosinusits or Recurrent Acute Sinusitis Failure of Aggressive Medical Therapy or Persistent Purulent Infection Most Common Disorders: Selective IgA Deficiency Hypogammaglobulinemia IgG Subclass Deficiency is Unclear HIV Patients ( 30-68%) Fungal Sinusitis Mycetoma Fungal Sinusitis “Fungus Ball” Usually in the Maxillary Sinus Treatment is Surgical Removal of the Lining Allergic Fungal Sinusitis An Allergic Reaction to Environmental Fungi Immunocompetent Host Thick Fungi and Mucin Accumulate Surgical Removal of the Allergen(Fungi) Fungal Sinusitis Chronic Indolent Sinusitis Generally outside the U.S. (Sudan, India) No Immune Deficiency Progresses from Month to Years Characterized by a Granulomatous Inflammatory Infiltrate Fulminant Fungal Sinusitis Immunocompromised Patients Immunodefeciency Disorders (Diabetes) Immunosuppressive Agents Can Result in Progressive Destruction of the Sinuses with Resulting Invasion of the Eye or Cranial Cavity Mucormycosis a common fungi Sinus Headache Clinical History: Primary Complaint is Headache Without Significant Nasal Symptoms – Migraine Headache Embedded In Other Bothersome Nasal Symptoms Evaluation of Nasal and Sinus Cavities Warranted Headache is a Minimal or Inconspicuous Complaint Rhinosinustis May Be Likely Sinus Headache Physical Exam: Nasal Exam Findings Which May Suggest Secondary Pathology: Inflammatory Changes (Allergy) Anatomic Abnormalities Purulent Nasal Discharge Testing: Imaging Can Be Useful – False Positive Results Sinus Headaches Sinus Disease As A Cause of Headache Has Been Ingrained Into The American Public Little Evidence to Support This Migraine Can Present With Facial Pain, Nasal Congestion and Rhinorrhea. In Clinical Studies Nearly 90% With Self-Diagnosed or Physician Diagnosed Sinus Headache Met The Criteria for IHS Migraine-Type Headaches. Most Responded To Triptan Interventions Sinus Headaches Specialist Referral Treatment 90% of Patients Can Be Treated and Cured of Sinusitis With Medical Therapy Surgical Treatment: For the Treatment of Anatomic Obstruction (Polyps,Septal Deviations) Recurrent Acute Infections CRS Non-Responsive To Medial Therapy Surgical Treatment Functions Endoscopic Sinus Surgery (FESS): All done through the nose Removal of Abnormal and Obstructive Tissue To Restore the Normal Drainage Pathways of the Sinuses Results in Removal of Less Normal Tissue Can Be Done as an Outpatient Surgical Treatment • Image Guided Surgery Three Dimensional View of the Surgical Field For Severe Cases or Patients Who Have Had Prior Surgery Requires a Planning CT BALLOON SINUPLASTY Questions?