The Effects of CPAP on Cardio
advertisement

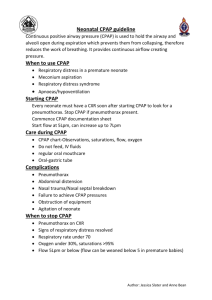
The Use of CPAP in Acute CHF Donald M. Pell M.D. FCCP The Effects of CPAP on Cardio-Respiratory Function I. Normal Physiology I. Normal Physiology • Normal respiratory effort is handled by the diaphragm. • Air is drawn into the lungs when the diaphragm contracts. • As diaphragm contracts, pressure falls in chest and rises in abdomen pressurizing venous blood to return to right heart, (the thoracic-abdominal pump). Normal Physiology (con’t.) • Air is drawn into lungs, reduced pressure in chest draws venous blood to right side of heart (pre-load). • The expanding lung acts as a pump, pools returning venous blood in lung circulation, decreases left heart filling. • Lung exhales, work is done by stretched elastic tissues and vessels, no effort. Normal Physiology (con’t.) • Lung expands/contracts, air spaces (alveoli) kept open by surfactant made by the lining cells. • Negatively charged, walls repel each other, preventing total collapse of the alveoli when in a near-empty air position. • This synchronized effort allows air/blood to flow through lungs, achieves CO2 transfer and acquires oxygen at same time. II. Abnormal Physiology Acute Heart Failure (Pulmonary Edema) Acute Heart Failure (Pulmonary Edema) • Most illness involves left heart. • Right heart is a receiving chamber, thin and distended accommodating returning blood volume. • Left heart 6 times thicker than right as it pumps higher pressures i.e., 120 systolic, 80 diastolic. Acute Heart Failure (con’t.) • With heart failure, stroke volume (number of cc’s blood/per beat) falls – to make up for decreased cardiac output, heart rate rises. • Increased rate/sympathetic tone . . . - Increases oxygen demand - Increases myocardial work Acute Heart Failure (con’t.) • Usual causes of left heart failure include: - Arterial sclerosis - Hypertension - Vascular Disease and/or - Cardiomyopathy . . . … alcohol … thyrotoxicosis … viral … familial Acute Heart Failure (con’t.) • Left heart is thick, can’t distend. • Right heart continues to pump making: - lungs become stiff/rigid, - lungs become harder to ventilate, - reduces gas space, - water fills air sacs, - gas transfer oxygen decreased, - O2 level falls. Acute Heart Failure (con’t.) • Therapies to improve left heart reduce pre-load . . . (blood getting to the heart) and therapies that reduce afterload (resistance to blood flow leaving the left heart). - Nitroglycerin and ACE Inhibitors • Drugs to reduce sympathetic tone (autonomic vasoconstriction/fluid retention). - Aldactone CPAP Types Some examples of CPAP Systems . . . Vitaid PulmodyneTM Boussignac O2-RESQTM Philips Respironics Mercury Medical® Flow-Safe TM WhisperFlow ® There are many types of CPAP systems available today. Some use flow generators, others do not. The new disposable CPAP systems are cost-efficient, lightweight, convenient and reliable. Most are available with accessories such as; masks, head straps, T-piece, filters, valves and connectors. Acute Heart Failure (con’t.) • CPAP Therapy - improves abnormal work-of-breathing, - corrects hypoxia, - decreases myocardial O2 consumption, - reduces pre-load/afterload, - decreases sympathetic tone reducing cardiac risk, and decreases cardiac arrhythmia. What is CPAP? (continuous positive airway pressure) • Pressurizing O2 with a mixture to lungs through sealed mask device with titratable flow: - Fast attainment of work reduction and cardiac stability. - Decreased need for intubation and possible consequences. - misplacement, - tissue damage/bleeding, - cardiac arrhythmia, - dental damage. What is CPAP? (con’t.) • Pressure/Flow generators no longer necessary . . . - disposable CPAP systems require no pressure/flow generator, only oxygen flow, - titratable from 2-1/2 cm H2O to 10 cm H2O, - Improved head straps, coaching, and attaining O2 saturation, - CPAP is transferred to E.R. along with O2 flow/pressure settings for continued continuity of care. What is CPAP? (con’t.) • CPAP? - It’s like blowing up a balloon and allowing it to inflate the lungs. - Set level of pressure is applied to raise airway pressure and expand alveoli. It will also restrict air flow out of lung (like pursed lip breathing). - Expiratory work done by elastic recoil of lung, doesn’t require muscle help once CHF improves. Respiratory Goals of CPAP . . . • • • • • • • Increased Alveoli gas volume, Increased PO2, Decreased work-of-breathing, Increased O2 transfer, Lower respiratory muscle oxygen requirement, Satisfying patient’s respiratory flow needs, Improving patient’s comfort/clinical status/level of consciousness. Cardio-Respiratory Effects of CPAP CPAP systems dramatically/beneficially affect pressure/flow. • Air is positively pressurized and pushed into airway reducing inspiratory muscle work, decreasing venous blood flow returning to right heart as venous flow has to be at higher level than pressure resisting blood return (CPAP). • Less blood pooling in lungs/less fluid transferred into air space. • Decreased sympathetic tone. • Decreased afterload on left heart. • Decreased cardiac heart rate. • Resulting in lowered cardiac work/O2 consumption/reduced cardiac arrhythmia risk. When to Use CPAP . . . • • • • • • • Can’t maintain O2 saturation @ 92%/4 liters, Respiratory distress increasing, Patient’s level of consciousness decreasing, Cardiac arrhythmia not responding to drugs, Respiratory Acidosis increasing (rising PCO2), Cardiac rate of 120+ not responding to oxygen therapy, Respiratory rate of 36+ not responding to oxygen therapy. Proper Use CPAP • Allow patient to hold device in place to feel improvement in inspiratory ease-of-breathing. • Once patient is comfortable, titrate pressure upward for desired results. • Proper mask fit/nasal fit. • Adjust head strap once patient is comfortable. • Stay with patient, coach on improvements attained. • Adjust flow for patient’s inspiratory flow rates. • A positive attitude/device can relieve consequences of CHF. Goals of CPAP • Attain O2 saturation of 92%, • Decrease work-of-breathing/improve patient’s respiratory status, • Decreased cardiac rate of 120 or less, • Decreased respiratory rate below 30, • Improved PCO2 level if elevated, • Improved cardiac arrhythmia, • Reduced need for in-the-field intubations, • Improved mental status/cooperation, • Leave CPAP equipment/settings with patient when transferred from transport to E.R. Contraindications of CPAP • Facial Trauma/fractures. • Recent gastric surgery. • Dense, copious respiratory secretions/frequent suctioning. • Patient unable to tolerate mask. • Respiratory arrest. • PCO2 greater than 50 in CHF patient/monitor (relative). • Near lethal cardiac arrhythmia (ventricular tachycardia, ventricular fibrillation). • Decreased level of consciousness. • Persisting vomiting. • Pneumothorax. Possible Side Effects of CPAP • Nasal bridge skin necrosis (rare). • Hypotension due to decrease in venous return (rare). • Claustrophobic (coaching/proper technique), may eliminate. What if Diagnosis is Incorrect? C.O.P.D. In spite of usual over-inflation of lungs . .. • • • • • CO2 is lowered, O2 saturation is improved, LOC improves as PCO2 falls, Respiratory effort is enhanced, CO2 production is decreased. In E.R. • Excess PO2 can be titrated downward (decrease pressure slowly), increased PCO2 and low O2 are corrected). • Due to dry state, low blood pressure occurs (rarely), to correct, use rehydration and adjust CPAP pressures downward. Asthma Using CPAP: • Reduction in inspiratory work. • Better expansion of previously collapsed alveoli with reduced CO2 level and increased O2 level. • Reduced need for intubation.