Research Seminar Slides - Charles Christoph Röhr
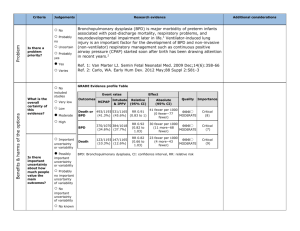
advertisement

How continuous positive airway pressure (CPAP) is currently being used – an overview C. C. Roehr, G. Schmalisch, R. Wauer Charité Universitätsmedizin Berlin Germany NCA/Hudson Mono-nasales Tubus CPAP F&P Bubble CPAP Beneviste valve „Kniewasser“ System Neo-Fit Infant-Flow driver Long and short binasal prongs NCA/Hudson Mono-nasal CPAP F&P Bubble CPAP „Kniewasser System How is CPAP being used neonatal medicine? Neo-Fit Infant-Flow driver Longe and short binasal prongs Use of CPAP in German, Austrian and Swiss neonatal units • for which clinical purpose? • when used as primary therapy? • what CPAP-system used? • mono- or bi-nasal? • flow and CPAP-level • differences between levels of care? • CPAP use in the delivery room Methods • Questionnaire study • German national survey and internatinal survey (FRG, A, Ch) • all maximum level NICU and paediatr. Hospitals • mailed questionnaire • telephone interview • Statistical analysis (Statgraph®) Methods Nation wide survey of all NICU (level 1-3) International (FRG, A, Ch) survey of all level 3 NICU Mailed questionnaire Postal reminder after 4 weeks Telephone interview Data-Analysis MS Excell / Statgraphics Results German survey Contacted institutions n = 274 Surveyed institutions Response 1st questionnaier n = 147 (53%) Reponse to questionnair Response reminder n = 127 (47%) Response to tel. contact Telphone contact n = 70 (26%) Roehr C et al. 2007 Results German survey Contatced institiutions n = 274 Surveyed institutions Response 1st questionnaire n = 147 (53%) Reponse to questionnair Response reminder n = 127 (47%) Response to tel. contact Telephone contact n = 70 (26%) positive answer n = 218 (79%) Roehr C et al. 2007 Results German survey Contatced institutions n = 274 Surveyed institutions Response 1st questionnaire n = 147 (53%) Reponse to questionnair Response reminder n = 127 (47%) Response to tel. contact Telephone contact n = 70 (26%) positive answer n = 218 (79%) Roehr C et al. 2007 No aswer n = 57 (21%) Characteristics of institutions Admissions per year* Primary paed. care Secondary paed. care Tertiary paediatric care Total <10 ventilator beds >10 ventilator beds n (Mean and (Range) 85 259 (201000) 75 (89%) 7 (11%) 110 312 (501000) 93 (85%) 16 (15%) 23 393 (180-1100) 6 (27%) 16 (73%) 218 *p = 0.014 GGkl1500g/LebendgebJahr*100 Patients < 1500g/year Box-and-Whisker Plot 10 8 6 4 2 0 Primary 1care hosp. Secondary care 2 tertiary 3 care hospital Institution Einrichtung p<0.0001 between institutions No sign. difference in CPAP use across institutions Guideline CPAP use CPAP post extubation CPAP – ADS 57 % 95 % 93 % n Primary paed. care 85 CPAP ApnoeaBradycardiaSyndrome 98 % Secondary paed. care Tertiary paediatric care p= 95 % 110 97 % 53 % 23 96 % 100 % 100 % 74 % 0,13 100 % 0,57 0,46 0,28 Mono-, bi-nasal, or both CPAP-systems? Differences between institutions not statist. significant Use of CPAP as commercial system, composite system or custom made Commercial system Composite Systems Custom made system Roehr C et al. Eur J Med Res 2007: 12; 139-44 CPAP generators used in German NICUs sonstige Fisher & Paykel Infant Star Leoni Bubble CPAPSystem F 120 B Christina 9% 26% F 120 M F 120 A 13% Stephanie 36% Roehr C et al. Eur J Med Res 2007: 12; 139-44 Babylog 8000 Leoni Infant Flow System (EME) Babylog 8000 Stephanie F 120 A Infant flowSystem driver Infant Flow F 120 M (EME) (EME) Christina F 120 B Bubble CPAP-System Infant Star sonstige Maximum tolerated CPAP 80 70 60 % 50 40 30 20 10 0 1 5 2 6 3 7 4 8 5 9 -12 CPAP in cmH CPAP in cm H20 2O Median 7 cmH2O Differences between institutions not statist. significant Frequency (%) Flow under CPAP 1 to 4 4.5 - 5.5 L/min 6-7 Median 6 L/min 8-9 Differences between institutions not statist. significant 2nd investigation: A survey of neonatal units of German speaking countries International survey FRG, A, CH Stepwise approach of tertiary neonatal units Units approached with 1st questionnaire 2nd questionnaire n = 249 100% n = 123 49% n = 25 10% Telephone interview Results: CPAP in DR O2- Blenders 97 Pulse oxymetry 97 Self-inflating bag 92 T-piece resuscitator 40 sust. inflations < 5sec 34 prol. inflations > 5sec 25 CPAP 4-5 cmH2O 76 Polyethylene foil 62 Hat / head cover 80 Late-clamping 43 0 10 20 30 40 50 60 70 80 90 100 in percent (%) *no statistical difference between regions, univ. or non-univ. neonatal units Summary • Wide spectrum of clinical appliactions – RDS – Apnoea-Bradycardia-Syndrome and – post-extubation • parallel use of low-flow (bubble) CPAP, high-flow and respirator generated CPAP • Heterogeneity of flow and CPAP-levels • CPAP in DR used with and without prolonged inflations Conclusion • Use of CPAP in German speaking countries is not standardized • We believe this may reflect gaps in knowledge on the potentials of CPAP, as well as lack of sound evidence for specific areas of CPAP therapy further clinical studies are needed. Educational opportunities to learn about CPAP should be widely offered.