Targeted therapies in
Gastroesophageal Malignancies
Dawn of a new era
Manish A. Shah, MD
Associate Professor of Medicine
Weill Cornell Medical College of Cornell University
New York-Presbyterian Hospital
Director, Gastrointestinal Oncology
Center for Advanced Digestive Care
Objectives
Discussion of abstracts:
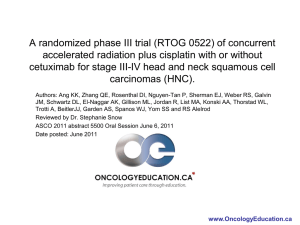
• LBA6 – Suntharalingam and colleagues
• RTOG 0436 – phase III study of chemo/RT (cisplatin
and paclitaxel) with and without cetuximab for
esophageal cancer treated without surgery
• LBA7 – Wilke and colleauges:
• RAINBOW – phase III study of paclitaxel with or without
ramucirumab in 2nd line gastric/GEJ adenocarcinoma
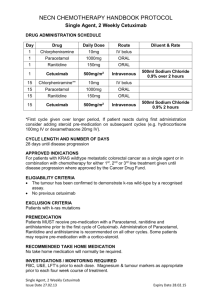
The Initial Report of RTOG 0436: A Phase III Trial evaluating
the addition of Cetuximab to Paclitaxel, Cisplatin, and
Radiation for Patients with Esophageal Cancer Treated
without Surgery
Suntharalingam M, Winter K, Ilson D, Dicker A,
Kachnic L, Konski A, Chakravarthy B, Anker C, Thakrar
H, Horiba N, Kavadi V, Deutsch M, Raben A, Roof
K,Videdic G, Pollock J, Crane C
Abstract LBA6 - Background
RTOG 0436 – Cetuximab in Esophageal CA
• Why paclitaxel / Cisplatin?
Cisplatin + Paclitaxel
with radiation was
equivalent to
cisplatin/FU + radiation,
but with less toxicity.
(enrollment 2001-2005)
Ajani J A et al. RTOG 0113: Phase II randomized trial of two nonoperative regimens of chemoradiation in localized esophageal
CA. JCO 2008;26:4551-4556
Abstract LBA6 - Background
RTOG 0436 – Cetuximab in Esophageal CA
• Context in the CROSS preoperative study
Eligibility: T1N1 – T2-3Nx (stage 1-3)
Treatment: Radiation 4140 cGy + weekly taxol (50 mg/m2) and
Carboplatin (AUC 2)
van Hagen P et al. Preoperative chemoradiotheapy for esophageal or junctional cancer. NEJM 2012;366:2074-84.
Abstract LBA6 - Background
RTOG 0436 – Cetuximab in Esophageal CA
• Why cetuximab?
– Cetuximab: a chimeric (mouse/human) monoclonal
antibody against epidermal growth factor receptor
(EGFR)
– EGFR expression in ~80% (30-90%) esophageal cancer,
~40% gastric cancer
– EGFR expression correlates with prognosis in
esophagogastric ACA and SCC
– KRAS mutations occur in ~2% (0-9%) of esophageal
cancers
Mukaida. Cancer 1991; Itakura. Cancer 1994; Yacoub. Mod Pathol 1997; Torzewski. Anticancer Res 1997; Koyama. J Cancer Res
Clin Oncol 1999; Lea. Carcinogenesis 2006
RTOG 0436: Overall Survival
100
• Well designed and
performed study,
2-Year
Rates:
44.0%
41.7%
Overall Survival (%)
75
(n=328)
50
• Reasonable
stratification
Stratified log-rank p-value =0.70
25
• No survival difference
Failed Total
RT+Chemo+Cetux 97 159 HR= 0.92 (0.70,1.21)
RT+Chemo
110 169
0
0
Patients at Risk
RT+Chemo+Cetux 159
RT+Chemo
169
3
6
9
12
15
18
Months from Randomization
139
158
124
141
108
121
94
102
82
83
65
68
21
24
54
54
51
49
Median follow-up for alive patients = 24.3 months (0.1-60.7)
Comment
• Cetuximab does not improve survival or response
when combined with chemotherapy for localized
unresectable esophageal cancer.
• Consistent with previous results in metastatic
disease.
Phase III studies
EGFR Ab inhibitors are metastatic disease
Comment
• Cetuximab does not improve survival or response
when combined with chemotherapy for localized
unresectable esophageal cancer.
• Consistent with previous results in metastatic
disease.
• These data are definitive.
• Would the results be different in a pre-operative
setting. Likely not!
Comment
• Why didn’t this work? (now or previously)
Are esophageal cancers driven by EGFR signaling?
TP53
CDKN2A
EYS
ARID1A
SMAD4
PIC3CA
EGFR mutations did not occur as top mutations. But it is more complicated –
EGFR amplification did occur frequently.
Dulak AM et al. Whole-exome and whole-genome sequencing of esophageal adenocarcinoma identifies recurrent driver events and
mutational complexity. Nat Genet. 2013;45(5):478-=86.
Comment
• What have we learned?
100
Overall Survival (%)
75
50
25
cCR
Residual Disease
0
0
3
6
Patients at Risk
cCR
70
Residual Disease 43
70
34
62
25
Failed Total
28 70
35 43 HR= 3.67 (2.22,6.07)
9
12
15
18
Months from Randomization
56
19
51
16
45
12
38
7
21
24
30
7
29
7
• Clinical response to chemo/RT is prognostic.
Implications:
Our best approach to improving survival in this
disease is to improve response to therapy.
– PET directed therapy
CALGB 80803: PET directed chemo + chemo/RT
– Targeted therapy
RTOG 1010: Trastuzumab with chemo/RT
– Improve our understanding of tumor biology
RTOG 0436: 85% tissue collected
LBA7
RAINBOW: A Global, Phase 3, Randomized, Double-Blind
Trial of Ramucirumab and Paclitaxel (PAC) Versus Placebo
and PAC in the Treatment of Metastatic Gastric or
Gastroesophageal Junction (GEJ) Adenocarcinoma
Following Disease Progression on First-Line Platinum- and
Fluoropyrimidine-Containing Combination Therapy
H. Wilke*
Eric Van Cutsem, Sang Cheul Oh, György Bodoky,
Yasuhiro Shimada, Shuichi Hironaka, Naotoshi Sugimoto,
Oleg Lipatov, Tae You Kim, David Cunningham, Atsushi Ohtsu, Philippe
Rougier, Michael Emig, Roberto Carlesi,
Kumari Chandrawansa, Kei Muro
*On behalf of the RAINBOW Investigators
RAINBOW: Study Design
1:1
S
C
R
E
E
N
R
A
N
D
O
M
I
Z
E
Ramucirumab 8 mg/kg day 1&15
+ Paclitaxel 80 mg/m2 day 1,8 &15
of a 28-day cycle
N = 330
Placebo day 1&15
+ Paclitaxel 80 mg/m2 day 1,8 &15
N = 335
Treat until
disease
progression
or
intolerable
toxicity
Survival and
safety
follow-up
•
Important inclusion criteria:
- Metastatic or loc. adv. unresectable gastric or GEJ* adenocarcinoma
- Progression after 1st line platinum/fluoropyrimidine based chemotherapy
• Stratification factors:
- Geographic region,
- Measurable vs non-measurable disease,
- Time to progression on 1st line therapy (< 6 mos vs. ≥ 6 mos)
* GEJ= gastroesophageal junction; gastric and GEJ will be summarized under the term GC
RAINBOW: Overall Survival
HR (95% CI) = 0.807 (0.678, 0.962)
1.0
Stratified log rank p-value = 0.0169
0.9
RAM + PAC
Patients / Events
330 / 256
Median(mos) (95% CI) 9.63 (8.48, 10.81)
0.8
Overall Survival Probability
0.7
6-month OS
12-month OS
0.6
72%
40%
0.5
PBO + PAC
335 / 260
7.36 (6.31,
8.38)
57%
30%
Δ mOS = 2.3 months
0.4
0.3
RAM+PAC
0.2
PBO+PAC
0.1
Censored
0.0
0
2
4
6
8
10
No. at risk
RAM + PAC
PBO + PAC
330
335
308
294
267
241
228
180
185
143
148
109
12
14
16
Months
116
81
78
64
60
47
18
41
30
20
24
22
22
13
13
24
26
6
5
28
1
2
0
0
Comment
• Well performed international study – kudos to
the investigators and to Lilly.
• Why did it work?
Avagast
Overall Survival : Cis/Cape +/- Bevacizumab
Survival rate
XP + Placebo
1.0
XP + Bev
0.9
0.8
HR = 0.87
0.7
95% CI 0.73–1.03
0.6
p = 0.1002
12.1
0.5
10.1
0.4
0.3
0.2
0.1
0.0
0
3
6
9
12
Study month
15
18
21
24
Bevacizumab plus CT for Advanced Gastroesophageal
Adenocarcinoma (GC): Combined U.S. experience*
Tumor Characteristics
US cohort
AVAGAST
Chemo + Bev arm
p value
n
%
n
%
Gastric
64
(41)
333
(86)
GEJ
92
(59)
54
(14)
Diffuse
42
(27)
176
(46)
Intestinal
Mixed
81
(52)
155
35
(40)
(9)
<0.0001**
Not reported
33
(21)
Liver metastasis
81
(52)
130
(34)
<0.0001
Site
<0.0001
Lauren's Classification*
*Data from 4 investigator initiated U.S. phase II studies of chemotherapy plus bevacizumab for the
treatment of metastatic/unresectable gastric cancer were pooled. Sites involved were: 1) Memorial
Sloan-Kettering Cancer Center, 2) Dana-Farber/Harvard Cancer Center, 3)Yale Cancer Center, and 4)
Stanford Comprehensive Cancer Center.
Smyth, et al. ASCO 2011 (Abstract 4056)
Patient characteristics by region
AVAGAST Study
Characteristic, %
Age
ECOG PS
Primary site
Disease status
Prior gastrectomy
Measurable lesion
Liver metastasis
Asia
Europe
Pan-America
<65
72
68
77
≥65
28
32
23
0–1
97
91
96
≥2
3
9
4
Stomach
94
78
84
GEJ
6
22
16
Metastatic
99
95
92
Locally advanced
1
5
8
Yes
32
23
27
No
68
77
73
Yes
73
88
77
No
27
12
23
Yes
27
37
42
No
73
63
58
There was an imbalance of >10% between the regions
*1 additional patient had an ECOG PS of 4
Avagast vs. Ramicirumab
Avagast
Rainbow
Study Design
1st line
2nd line
Backbone
chemotherapy
Cisplatin/ capecitabine
Paclitaxel
Demographics
N = 774
N = 665
Asia
376 (49%)
223 (33.5%)
Non-Asia
398 (51%)
442 (66.5%)
Asia
12.1 13.9 mo
HR 0.97 (0.75-1.25)
10.5 12.1 mo
HR 0.99 (0.73-1.34)
Non-Asia
7.3 11.4 mo
HR 0.67 (0.52-0.88)
5.9 8.5 mo
HR 0.73 (0.59-0.91)
Asia
5.6 6.7 (HR 0.92)
2.8 5.5 (HR 0.63)
Europe
4.4 6.9 (HR 0.71)
Pan-America
4.4 5.9 (HR 0.65)
Results OS
Results PFS
2.9 4.2 (HR 0.64)
Avagast vs. Ramicirumab
Avagast
Rainbow
Study Design
1st line
2nd line
Backbone
chemotherapy
Cisplatin/ capecitabine
Paclitaxel
Demographics
N = 774
N = 665
Asia
376 (49%)
223 (33.5%)
Non-Asia
398 (51%)
442 (66.5%)
Asia
12.1 13.9 mo
HR 0.97 (0.75-1.25)
10.5 12.1 mo
HR 0.99 (0.73-1.34)
Non-Asia
7.3 11.4 mo
HR 0.67 (0.52-0.88)
5.9 8.5 mo
HR 0.73 (0.59-0.91)
Asia
5.6 6.7 (HR 0.92)
2.8 5.5 (HR 0.63)
Europe
4.4 6.9 (HR 0.71)
Pan-America
4.4 5.9 (HR 0.65)
Results OS
Results PFS
2.9 4.2 (HR 0.64)
Avagast vs. Ramicirumab
Avagast
Rainbow
Study Design
1st line
2nd line
Backbone
chemotherapy
Cisplatin/ capecitabine
Paclitaxel
Demographics
N = 774
N = 665
Asia
376 (49%)
223 (33.5%)
Non-Asia
398 (51%)
442 (66.5%)
Asia
12.1 13.9 mo
HR 0.97 (0.75-1.25)
10.5 12.1 mo
HR 0.99 (0.73-1.34)
Non-Asia
7.3 11.4 mo
HR 0.67 (0.52-0.88)
5.9 8.5 mo
HR 0.73 (0.59-0.91)
Asia
5.6 6.7 (HR 0.92)
2.8 5.5 (HR 0.63)
Europe
4.4 6.9 (HR 0.71)
Pan-America
4.4 5.9 (HR 0.65)
Results OS
Results PFS
2.9 4.2 (HR 0.64)
Biomarkers- pVEGFA and NRP
Candidate Biomarkers for Bevacizumab Efficacy in
Gastric Cancer
Van Cutsem E [Shah MA]. JCO 2012;30:2119-2127
Implications
• Targeting the angiogenesis pathway in
gastric/ GEJ adenocarcinoma is now
validated
• Ramicirumab + paclitaxel is a viable, safe,
effective treatment option following 1st line
therapy.
• Is VEGFR2 specific inhibition any different
than blocking VEGF-A?
What have we learned
• Disease biology is important, as shown by
gastric cancer heterogeneity.
Immune
SNPs
IL1, IL4, etc.
Family History:
CDH1
MMR
APC
TP53
Genetic
Risk
Environment
Behavior
Tobacco use/ diet (salt)
(fruits/vegetables)
H. Pylori
cag A strain
Are we at the
Dawn of a new era?
Shah MA. Nat Rev Clin Oncol 2014;11:10-11.
Are we at the
Dawn of a new era?
Pathway
MET
HER2
EGFR
Angiogenesis
Agent
Clinical Trial
Randomization
Ornartuzumab
METGASTRIC
Rilotumumab
RILOMET
FOLFOX +/ornatuzumab
ECX +/- rilotumumab
Pertuzumab
JACOB
XP-T +/- pertuzumab
Trastuzumab
HELOISE
TDM-1
GATSBY
Lapatinib
TyTAN
Panitumumab
REAL-3
XP-T (standard) vs.
XP-T (high dose)
TDM-1 vs taxane
(2nd line)
Paclitaxel +/- lapatinib
(2nd line)
EOX +/- panitumuamb
Cetuximab
EXPAND
XP +/- cetuximab
Ramucirumab
REGARD
Ramicirumab
RAINBOW
Ramucirumab vs. BSC
(2nd line)
Paclitaxel +/Ramucirumab (2nd line)
Regorafenib
INTEGRATE
Regorafenib vs BSC
(2nd line)
Patients
800
450
780
400
412
261
574
904
355
665
150
Targeted Successes
Target
Study
Setting
Clinical Benefit
HER2
TOGA
1st line HER2
positive
HR 0.74
(2.7 month)
VEGFR2
REGARD
2nd line
monotherapy
HR 0.78
(1.4 month)
RAINBOW
2nd line
combination
HR 0.81
(2.3 month)
Dawn of …. more of the same?
Target
Study
Why does it
work?
Why does it not?
HER2 drives
tumor growth and
proliferation
?
HER2
TOGA
VEGFR2
REGARD
Blocks VEGFR2
?
RAINBOW
Blocks VEGFR2
?
Angiogenesis
Bevacizumab
Inhibits VEGF-A
?
Mictrotubules
Taxanes
Arrests cell
division
?
DNA Synthesis
Fluoropyrimidines
Stops DNA /RNA
synthesis
?
DNA Damage
Platinum
Accumulation of
DNA damage
?
We are in a New Era !
• Greater emphasis on obtaining tissue and
biospecimens
• Greater tools at our disposal
– [put your – omic here]
Focus our efforts on
understanding how therapy works
understanding why therapy doesn’t work
why therapy stops working
That is our
next move….

![Rainbow Sandals[1]](http://s2.studylib.net/store/data/005415944_1-86d746c06518ebd8de8a03e56a4931b4-300x300.png)