RT vs. RT-CHX
advertisement
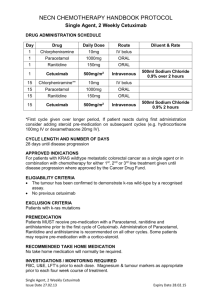
Protokolle und Indikationen für die kombinierte Radiochemotherapie Wilfried Budach Düsseldorf Meta-analysis of 93 randomized trials (Pignon et al. 2009) Individual data of 17,346 patients Meta-analysis: Induction TPF vs. Induction PF before RT or RT-CHX Hitt et al. ESMO 2008 MARCH- Meta-analysis on early death (<=day 90) Pignon et al. Radiother Oncol Web figures 2009 Meta-analysis by tumor site (Blanchard et al. Radiother Oncol 2011) Meta-analysis of 93 randomized trials (Pignon et al. 2009) (no head to head comparisons of different chemotherapy schedules) death ARO/-AHMO 04-01 TRIAL Overall Survival + 5FU + 5FU V. Budach, ARO 04-01 Trial, ESTRO 2010 Concomitant Chemoradiation: Which schedule should be used? • Many consider 100 mg/m² cisplatin (d1, 22, 43) standard • Fractionated cisplatin e.g. 30-40 mg/m² weekly or 20mg/m² d1-5 + d29-33 seem to be equally effective and less toxic • Mitomycin C (10 mg/m² weeks 1+5) + 5-FU (600 mg/m² CI d1-5 + d29-33) has also been shown to be effective • Carboplatin 70-75 mg/m² + 5-FU 1000 mg/m² CI d 1-4 + d29-33 of RT is also an option • The exact value of aditional 5-FU is unknown Medikamentöse Tumortherapie der Kopf-, Hals-Tumoren W. Budach, Düsseldorf Meta-analysis of 93 randomized trials (Pignon et al. 2009) Age dependence death Meta-Analysis : Which fractionation is the best? End Point: Locoregional Recurrence Hyperfractionation Accelerated fractionation Very accelerated fractionation (with moderate dose escalation) vs. conventional fractionation without decreased total dose vs. conventional fractionation with decreased total dose vs. conventional fractionation Bourhis, Lancet 2006 Meta-Analysis : Which fractionation is the best? Bourhis, Lancet 2006 End Point: Overall Survival Hyperfractionation Accelerated fractionation Very accelerated fractionation (with moderate dose escalation) vs. conventional fractionation without decreased total dose vs. conventional fractionation with decreased total dose vs. conventional fractionation RTOG 0129: Objective & Study Design Do we need accelerated RT, if RT is combined with concurrent CHX? 72 Gy + 200 mg/m² Cisplatin 70 Gy + 300 mg/m² Cisplatin Does 100 mg/m² cisplatin compansate for 1 week longer overall treatment time? RTOG 0129: Intent to treat analysis Kian Ang et al. 2010 Toxicity in random. H&N trials: RT vs. RT-CHX (grade >=III) “Older random trials” on concurrent Chemoradiation Toxicity in random. H&N trials: RT vs. RT-CHX (grade >=III) “newer random trials” on concurrent Chemoradiation Multivariate analysis with grade 2–4 RTOG swallowing dysfunction at 6 months as primary endpoint n=529 Langendijk et al. Radiother Oncol 2009 Locally advanced head and neck cancer: RT vs. RT + cetuximab RT (n = 213) Stadium III und IV nicht metastasierendes SCCHN (n = 424) R Cetuximab + RT (n = 211) Initialdosis 400 mg/m² (1 Woche vor RT) dann 250 mg/m² + RT (Wochen 2 – 8) Stratifiziert durch: • • • • KPS Lymphknotenbeteiligung Tumor Stadium RT Regime • • Primärer Endpunkt Dauer der lokoregionären Kontrolle Sekundäre Endpunkte • Gesamtüberleben (OS) Progressionsfreies Überleben (PFS) • Ansprechrate (RR) • Sicherheit Bonner et al., N Engl J. Med 2006; 354: 567 – 578. Locally advanced head and neck cancer: RT vs. RT + cetuximab locoregional control Bonner et al. NEJM 2006 overall survival Locally advanced head and neck cancer: RT vs. RT + cetuximab Overall Survival: Update with 5 years follow up Bonner et al Lancet Oncol 2010 Locally advanced head and neck cancer: RT vs. RT + cetuximab Overall survival and cetuximab induced skin rash BonnerBonner et al Lancet Oncol 2010 et al, ASTRO 2008 Locally advanced head and neck cancer: RT vs. RT + cetuximab Foster plot: Update with 5 years follow up Bonner et al Lancet Oncol 2010 Radiotherapy vs. radiotherapy + cetuximab: adverse events Bonner et al. NEJM 2006 RT + Cetuximab: Radiodermatitis W. Budach et al. NEJM 2007 RT + Cetuximab: Radiodermatitis EORTC questionnaire (Giro, Radiotherapy and Oncology 2009) Recommended schedules for simultaneous chemo(bio)radiation Best evidence (2 or more randomized trials) •Cisplatin 100 mg/m² d 1,22, and 43 of RT •Cisplatin 30-40 mg/m² weekly •Cisplatin 12-20mg/m² + 5-FU 600 mg/m² CI d 1-5 and 29-33 of RT •Mitomycin C 10mg/m² d 5 + 36 + 5-FU 600 mg/m² CI d 1-5 of RT Good evidence (at least 1 large randomized trial of high quality) Carboplatin 70-75 mg/m² + 5-FU 1000 mg/m² CI d 1-4 + d29-33 of RT Cetuximab 400 mg/m² d-8 + weekly Cetuximab 250 mg/m² during RT Some evidence (at least 1 randomized trial) Cisplatin 20mg/m² d 1-5 and 29-33 of RT Cisplatin 6 mg/m² on all RT days Carboplatin weekly AUC 1.5 during RT Carboplatin 25 mg/m² on all RT days Mitomycin 10-15 mg/m² day 1 of RT 5-FU 1000 mg/m² CI d1-4 and d 29-32 of RT Locally advaned HNC: Treatment Options Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Kian Ang et al. ASCO 2011 Postoperative Chemoradiation vs. Radiation Locoregional tumor control pT3 R1 or pT4 or ECE or ≥ 3 LN+ pT3 or pT4 or LN+ R1 or ≥ 2 LN+ or ECE 45% ECE Close margin ? 57% ECE Close margin: 29% 55% ECE Close margin 10% ARO 96-03 Fietkau et. al. ASCO 2006 EORTC Bernier et. al. NEJM 2004 RTOG Cooper et. al. NEJM 2004 Meta-analyses: EORTC and RTOG studies adjuvant RT vs. RT-CHX J. Bernier et al. 2005 Meta-analyses: EORTC and RTOG studies adjuvant RT vs. RT-CHX Subgroup: close margin (<5 mm) or extracapsular extention Overall survival J. Bernier et al. 2005 Meta-analyses: EORTC and RTOG studies adjuvant RT vs. RT-CHX Subgroup: R0 (≥5 mm) and no extracapsular extention Overall survival J. Bernier et al. 2005 Conclusion: adjuvant RT vs. RT-CHX Concurrent chemoradiation ist standard of care for high risk patients (ECE or close margin [<5 mm]) Overall survival in this high risk group is still below 50% at 5 years. DFS at 5 years is 36% EGFR antagonist have not been show to be effective in the adjuvant setting How much surgical safety margin is needed? Langendijk et al. Cancer 2005 Chemotherapy schedules in combination postoperative radiotherapy EORTC Cisplatin 100 mg/m² days 1,22, and 43 of radiotherapy RTOG Cisplatin 100 mg/m² days 1,22, and 43 of radiotherapy ARO Cisplatin 20mg/m² days 1-5 and 29-33 of radiotherapy + 5-FU 600 mg/m² CI days 1-5 and 29-33 of radiotherapy Radiotherapy: 5x2 Gy per week to 64 Gy (ARO) - 66 Gy (RTOG /EORTC) Acute toxicity: adjuvant RT vs. RT-CHX Grade III/IV mucositis RT+ Cisplatin RT p EORTC post –OP 41% 21% 0.001 RTOG 30% 18% 0,003 21% 13% 0.038 post –OP ARO* post –OP Spätnebenwirkungen Grad III/IV jeweils tendenziell erhöht (nicht signifikant) *Cisplatin + 5FU Impact of HPV-status on outcome of different treatment strategies in head & neck cancer Locoregional control Overall survival DAHANCA: RT +/- nimorazole (?) Overall survival n=131 CHAIR OP +: RT Overall survival RTOG: RT + cisplatin TAX 324: PF/TPFRT + carboplatin HPV 16 Promotes tumor induction by: • E6 and E7 gene maybe integrated into the human genom • E6 decreases p53 function resulting in genetic instability • E7 inhibits pRB resulting in loss of cell cycle control • upregulation of p16 Impact on radiation response: (Human cervical cancer cell line): • Transfection with E6 enhances radiation sensitivity Shin et al. Int J Radiat Biol. 2010 HPV pos. tumors do not have p53 mutations Stransky Science 2011 HPV/p16: DAHANCA 6&7 trial CF vs. AF Locoregional tumor control Lassen et al. Radiother Oncol 2011 Locally advanced head and neck cancer: RT vs. RT + cetuximab Foster plot: Update with 5 years follow up Bonner et al Lancet Oncol 2010 Kian Ang et al. ASCO 2011 Locally advanced unresected head and neck cancer • Concurrent Chemoradiation remains the standard of care • Concurrent Cetuximab and radiotherapy is an also an option • Induction TPF remains investigational • Accelerated RT is probably not needed in case of concurrent CHX • HPV/p16 positive head and neck cancer are a distinct entity, however, it is unknown whether different treatments should be offered for HPV positive and HPV negative disease • Future trials should test different treatment strategies for HPV/p16 positive and negative tumors