Traumatic Hemorrhagic Shock
and
Massive Transfusion Protocols
in Children
Philip C. Spinella, MD. FCCM
Associate Professor, Department of Pediatrics
Critical Care Translational Research Program Director
Washington University in St Louis
Epidemiology
• Trauma most common cause of death
– Children > 1 year of age in US
• Hemorrhage most common cause of preventable death
– 66-80% of preventable deaths are from hemorrhage
• Hemorrhagic death occurs fast – 6-12 hours
• Prevention of early death from hemorrhage - important
– Greatest Impact on Survival
• Objective: Incidence, association with mortality
– Shock and coagulopathy
• Retrospective: Combat Support Hospitals
– 744 children in Iraq and Afghanistan from 2002-2009
• Coagulopathy and Shock
– INR ≥1.5
– Base deficit (BD) ≥6.
Coagulopathy
27% (202/744) of patients presented w/ coagulopathy
Shock
38.3% (285/744) of patients presented with early shock
Adjusted Analysis
Table 3. Logistic regression results for in-hospital mortality
Variable
ISS
Coagulopathy
Shock
GCS
OR (95%Cl)
1.1 (1.1-1.1)
2.2 (1.1-4.5)
P value
<0.001
0.025
3.0 (1.1-7.5)
0.85 (0.80-0.91)
0.019
<0.001
Coagulopathy & shock, OR =3.8 (95% CI 2.0-7.4), (p<0.001)
PEDIATRICS Vol. 127 No. 4 April 1, 2011 pp. e892 -e897
Results
• 707 patients from the derivation set and
• 1101 patients in the validation set.
Table 2. Multivariate Logistic Regression for Mortality
Variable
Beta
Odds Ratio
P Value
Base Deficit
0.131
1.15 (1.1-1.2)
<0.001
INR
0.782
2.19 (1.5-3.3)
<0.001
Glasgow Coma Scale
-0.195
0.82 (0.78-0.87)
<0.001
INR, International Normalized Ratio
Results
• Pediatric “BIG” score
• (Base Deficit + (2.5xINR) + (15-GCS)
• AUC for derivation and
validation datasets
– 0.89 (95% CI 0.83-0.95)
– 0.89 (95% CI 0.87-0.92)
Grade V liver injury has a 76% mortality in
academic Level 1 Trauma Centers
DCR
• INDICATION: LIFE THREATENING INJURY
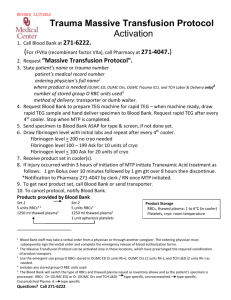
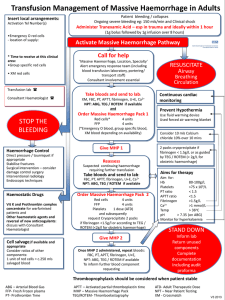
Massive Transfusion Protocol
MTP Principles
• Rapid surgical control
• Avoid overuse of crystalloids to minimize dilutional coagulopathy
• Continuously monitor patient temperature
• Avoid and treat hypothermia (use fluid warmer and Bair hugger if needed)
• Avoid and treat acidosis as needed; (pH<7.2 treat with bicarbonate or THAM)
• Treat low ionized calcium for hemostatic and hemodynamic effects
Laboratory evaluation upon admission
I stat: blood gas, lactate, Hb, ionized calcium and electrolytes, INR/PT.
Laboratory: Type & Screen, CBC, Fibrinogen, TEG (if available) – STAT
Laboratory Evaluation q hour until MTP stops
I stat: blood gas, lactate, Hb, ionized calcium and electrolytes, INR/PT.
Laboratory: CBC, Fibrinogen, TEG (if available) – STAT
PEDS MTP
18
Adjunctive Therapies
• Fibrinogen concentrates
– 30-50 mg/kg
– Fibrinogen concentration or TEG based
• Prothrombin complex concentrates
– Factors II, IX, X
– Factors II, VII, IX and X, Protein C and S – FDA IND
• Anti-fibrinolytics
– Tranexamic Acid (TXA)
• rFVIIa
CRASH-2 Trial
• Clinical Randomization of an Antifibrinolytic in Significant
Hemorrhage (Lancet, 2010)
– Prospective of 20,211 patients
– Multicenter (270 Hospitals)
– Multinational (40 Nations)
– Randomized, Blinded, Placebo-controlled
• One gram tranexamic acid over ten minutes followed by one
gram tranexamic acid given over eight hours
• Normal saline placebo
CRASH-2 Trial
• Inclusion Criteria:
– Adult Trauma victim
– Systolic blood pressure less than 90 mmHg
– Heart rate greater than 110
– Deemed to be at risk of significant
hemorrhage
CRASH-2 Trial
• Endpoints:
– Primary: In-hospital death within four weeks of injury
– Secondary
• Vascular occlusive events
• Surgical interventions
• Blood Transfusions
• Total units of blood transfused
CRASH-2 Trial- Results
• Decreased mortality:
• All-comers, 14.5% vs. 16.0% (p=0.0035)
• Deaths from bleeding, 4.9% vs. 5.7% (p=0.0077)
CRASH-2 Trial- Results
• Treatment ≤1 h from injury reduced risk of death due to
bleeding
– 5.3% in TXA vs 7.7% in placebo
– RR 0.68, (95% CI 0.57–0.82), (p<0.0001)
• Treatment from 1- 3 h also reduced risk of death due to
bleeding
– 4.8% vs. 6.1%
– RR 0.79, (0.64–0.97) (p=0.03).
• Treatment > 3 h increased the risk of death due to bleeding
– 4.4% vs. 3.1%,
– RR 1.44, (1.12–1.84), (p=0.004)
MATTERs Study
• Military Application of Tranexamic Acid in Trauma
Emergency Resuscitation (Arch Surg, 2012)
– Retrospective, observational of:
• 896 Combat-injured patients (both soldiers and
nationals) presenting to Camp Bastion Surgical
Hospital in Afghanistan
• Requiring a minimum transfusion of one unit
packed red blood cells
MATTERs Study
• Endpoints:
– Primary: 24-hour, 48-hour, and in-hospital mortality
– Secondary:
• Transfusion requirement
• Correction of PT and PTT between admission
and ICU
• Thromboembolic events
MATTERs Study
• Results (896 patients, 293 receiving TXA):
– Greater injury severity in TXA-treated group
• (ISS 25.2 vs. 22.5, p<0.001)
– Greater transfusion requirement in TXA-treated group
• (All products)
• Decreased Mortality in TXA treated:
• 48-hour (11.3 vs. 18.9%, p=0.004)
• In-hospital (17.4 vs. 23.9%, p=0.030)
– Reduction in hypocoagulability in TXA-treated group
from ED to ICU
MATTERs Study
• Thromboembolic events increased with TXA:
• PE
– (8 vs. 2, p=0.001)
• DVT
– (7 vs. 1, p=0.001)
Should TXA be used in Peds
MTPs?
• No evidence at all in children
• Adult data appears supportive
• Standard in Adult MTPs
• Reasonable to add
• Reasonable to wait for additional data
Fibrinogen Concentrates
• Provide high amount of fibrinogen rapidly
• Not frozen, rapidly reconstituted and given
• High cost
• No comparative data with cryoprecipitate in
trauma patients
Goal Directed Hemostatic
Resuscitation
• Hemostatic Resuscitation = 1:1:1
• Goal directed hemostatic resuscitation
– 1:1:1 that is tailored to patients needs
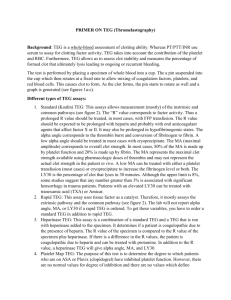
Thromboelastography (TEG)
• Whole blood test
– Plasma-platelet interaction
• Patient temperature
• Functional measurement of
– Clot initiation, amplification,
propagation, lysis
• TEG system
– Laboratory based
– Point of care
– Remote - networked
TEG
Parameter
Summary
TEG Parameter Summary
Back to the Future
With Whole Blood ?
Whole Blood Availability
• Classic teaching is that Platelets stored at 4C are
non functional
• Current data indicates IMPROVED function
• If whole blood can be stored for 10 days at 4C.
– Improved hemostatic effects in vivo
• Increase clinical utility significantly
Average ± SEM ADP-, collagen-, ASPI-, and TRAP-6-stimulated aggregation in WB stored at
4º C versus 22º C (p<0.001 for all four agonists by repeated measures ANOVA).
Pidcoke,H.F.,
Pidcoke, Heather, Transfusion. 2013 Jan;53 Suppl 1:137S-49S.
Manno - Methods
• Prospective double-blinded study
– 161 children requiring cardiac surgery
• Patients were randomized to
– Warm FWB (< 6 hours at 20 degrees C)
– Cold FWB (24 - 48 hours at 4-6 C)
– Reconstituted whole blood (1:1:1)
• (RBCs ≤ 5 days of storage, FFP, and platelets).
Manno CS, et al. Blood 1991;77:930-6.
Manno - Results
• Patient groups similar
– Sex and Age
– Surgical severity score
– By pass and circulatory arrest time
– # requiring circulatory arrest
Manno - Results
Warm FWB
Cold FWB
Recon Blood
(1:1:1)
P value
24 hr blood loss (ml/kg)
50.9 (±9)
44.8 (±6)
74.2 (±9)
0.03∞
24 hr blood loss (ml/kg)
< 2 yrs
52.3 (±11)
51.7 (±7.4)
96.2 (±11)
0.001§
PTT (30 min)
38.2 (±1.1)
39.7(±3.4)
43.3 (±1.8)
0.06
Fibrinogen (mg/dl)
202 (±5.4)
195 (±5.6)
184 (±4.8)
0.07
PLT aggregation
(30 min)
∞ cold vs recon
§ warm and cold vs recon
Manno CS, et al. Blood 1991;77:930-6.
most reduced
ADP, epinephrine, collagen
0.02
Warm FWB Benefits & Risks
• Benefits
– Less dilutional effect than components
• Less anti-coagulants and preservatives1
– More functional fresh product 2
– No storage lesion (adverse effects) of RBC
• Risks
– Infectious, GVHD, WBC mediated
1 Spinella PC, J Trauma. 2009;66:S69-76
2 Manno CS. Blood 1991;77:930-6.
Cold Whole Blood Trials
• Liver Transplant
• Burn
• Trauma
Case Example
Intraoperative Hemorrhagic Shock
• A 9 year old 20 kilogram male,
who previously underwent a right
nephrectomy and pulmonary
resection for Wilms tumor,
presented one year later with a
new lesion in the right lobe of his
liver
Figure 1: CT scan demonstrating coronal and
sagittal images of liver tumor
Case Example
• The patient was taken to the operating room (OR) and
a right hepatectomy was performed
• Due to severe intra-operative bleeding the MT
protocol was activated
Case Example
• During the 4 hours that the MT protocol was activated,
a total of 10 units RBCs, 14 units FFP, and 15 units of
platelets were transfused. (20 kg child)
• With EBL of over 4 liters no laboratory evidence of a
metabolic acidosis or shock indicated by normal base
deficit values
Case Example
• Upon admission to the (ICU)
• After receiving an intraoperative total of 13,100
milliliters (ml) of blood products
– (8 blood volumes)
• And 4,500 ml of normal saline
• Patient had no physical evidence of pulmonary
edema or anasarca.
Case Example
• Patient had no physical evidence
of pulmonary edema or anasarca.
• PEEP of 5 with Fi02 30%
• Extubated in AM
Implementation of MTP via
High Fidelity Simulation
• Improves identify systems issues
• Builds confidence
• Reinforces concepts for high risk low
frequency event
• Lab based vs Bedside scenarios
Conclusion
• Coagulopathy and shock are common
• Associated with high incidence of death
• Prospective trials of resuscitation are needed
in pediatric trauma patients
Conclusion
• Rapidly identify risk of shock and coagulopathy
• DCR concepts can be applied in children
• MTP helpful to reduce variation and
standardize care
• Goal Directed Therapy
– TEG/ROTEM ?
• Once bleeding stops – transfusion stops
Thanks to my
Band of Blood Brothers
John Holcomb
Charles Wade
Jeremy Perkins
Kurt Grathwohl
Alec Beekley
Jim Sebesta
Lorne Blackbourne
Matt Borgman
Thank you
Spinella_P@kids.wustl.edu
Philip C. Spinella, MD. FCCM
Associate Professor, Dept Pediatrics
Critical Care Translational Research Program Director
Washington University in St Louis
Component Therapy vs Fresh
Whole Blood
Component Therapy:
1U PRBC + 1U PLT + 1U FFP + 10U Cryo
660 COLD mL
•Hct 29%
•Plt 87K
•Coag activity 65%
•750 mg fibrinogen
•Armand & Hess, Transfusion Med. Rev., 2003
FWB:
500 mL Warm
Hct: 38-50%
Plt: 150-400K
Coags: 100%
1500 mg Fibrinogen
Standard Amounts of
Anti-coagulants and Additives in
Reconstituted Whole Blood vs Whole Blood
Component Therapy per Unit:
6 X RBC (AS-5) 6 X 120 ml = 720ml
6 X FFP
6 X 50 ml = 300ml
1 X aPLT
1 X 35 ml = 35ml
Total =1055ml
Whole Blood per Unit:
6 X 63ml = 378ml
Total: 378ml
There is 3 times the volume of anticoagulant and
additives with reconstituted whole blood from
components compared to whole blood
• Study of 455 transfused children in PICUs
• Prospectively collected data from a RCT
• One or more units of RBCs > 14 days of
storage was independently associated with
increased risk of new or progressive MODS
• Odds ratio = 2.3 (1.2-4.2), (p<0.05)




![Electrical Safety[]](http://s2.studylib.net/store/data/005402709_1-78da758a33a77d446a45dc5dd76faacd-300x300.png)