Testicular Pain & Testicular Masses
advertisement

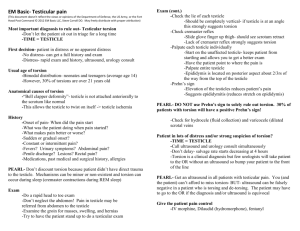
Evaluation of Testicular Disorders Richard E. Freeman MD MPH 2013 Lock Haven University Section 1 TESTICULAR EVALUATION Testicular Anatomy History Age of Patient helpful in limiting differential and determining responsible organisms : Nature of Pain: Sexual History Associated constitutional symptoms Associated urinary symptoms Severity Quality Radiation Alleviating/Aggravating factors Dysuria, frequency, hesitancy Discharge- etc Other Activities involved with: Sports-lifting, trauma Physical Exam Always complete GU: - be systematic Inspection- entire perineum- over, under, and beside Skin- cysts, ulcers, erythema/rash, parasites MassesPalpation Inguinal- hernias, masses, nodes Scrotum- Cord, Epididymis, Testes Penile shaft – palpate from bulbous to tip- masses tenderness ulcers Milk the shaft – discharge- Examine urethral meatus Rectal Hemorrhoids Prostate Masses Occult blood Abdominal Exam - Complete ?? Parotids Diagnostic Studies Urinalysis Urethral Discharge Gram Stain Culture PCR (Chlamydia/GC) Ultrasound Doppler Ultrasound Testicular Scan Doppler Ultrasound Diagnosis Appearance on U/S Normal testis Normal blood flow Testicular Torsion Absent or decreased blood flow Epididymitis/Orchitis Increased blood flow Appendiceal Torsion Normal blood flow Section 2 THE PAINFUL TESTICAL Case 1 A ten year old male presents to your clinic complaining of acute testicular pain while playing outside this afternoon. There is no history of trauma. He is afebrile and denies any recent symptoms of viral illness. On physical exam you note a tender right testicle that has a transverse lie in the scrotal sac. Elevating the testicle exacerbates symptoms. TESTICULAR PAIN: Differential Diagnosis Epididymitis/Epididymo-Orchitis Orchitis Testicular Torsion Torsion Torsion of Testicular appendix Torsion Testicle Severe pain - abrupt onset Possibly previous history of similar episode that resolved Absence of cremasteric reflex on affected side suggestive of torsion High riding testicle with transverse lie of testiclesuggests torsion Prehn’s sign- lack of pain relief with testicle elevation Torsion Testicle Occurs due to anatomic defect in scrotal development- Tunica Vaginalis compltely surrounds the testes and possibly the cord. No attachment of the Tunica vaginalis to the wall of the scrotum. Allows Testes to “swing freely “Bell-Clapper deformity” Two variations Intravaginal Torsion Extravaginal Torsion-Exclusively in neonates Torsion Testicle Incidence- 1:4000 males before age 25 TESTICULAR TORSION DIAGNOSIS: High degree of suspicion CLINICAL DIAGNOSIS Blood Flow: ULTRASOUND - color doppler Radionucleotide Torsion Testicle REPRESENTS SURGICAL EMERGENCY Requires immediate orchidopexy Contralateral side should be repaired at the same time Testicular Salvage rates < 6 hours – 90-100% salvage rate 12-24 hours – 20-50% > 24 hours – 0-10% Torsion Testicle Differential includes Appendiceal torsion Orchitis Epididymitis Appendiceal Torsion Onset of Symptoms: Age Subacute Prepubertal Tenderness Localized to upper pole UA Negative Cremasteric reflex Positive Treatment Bed rest/scrotal evalvation Surgical Torsion of Testicular appendix Appendix Testes Appendix Epididymis Remnant of Mullerian duct (92%) “Blue dot” sign More common in children than testicular torsion Remnant of Wolffian duct (23%) Present as Subacute pain Absence of systemic/Urinary tract symptoms Blue Dot sign Epididymitis DEFINITION: Inflammation, Pain, Swelling of epididymis Acute: Symptoms usually lasting < 6 weeks Chronic: Symptoms usually lasting > 6 weeks May be acute sub-acute chronic EPIDEMIOLOGY: Most common cause of acute scrotal pain Age: 16-30 y/o & 51-70 y/o Incidence parallels incidence of Chlamydia & GC Epididymitis ETIOLOGY: Retrograde infection from the urinary tract. Sexually active – Chlamydia, Gonorrhea, E.coli Older men and children- E.coli Non-infectious – post surgery, drugs SIGNS/SYMPTOMS: Scrotal pain- slow onset +- Dysuria, frequency, Discharge, Fever Tenderness and swelling epididymis Epididymitis Natural History/Complications Abscess Epididymis and testicular infarction Chronic inflammation/disability EPIDYDIMITIS Diagnostic Studies Urinalysis Urine Culture May reveal pyuria Responsible organisms Urethral Swab Gram Stain Culture PCR-Gonorrhea/Chlamydia Epididymitis Treatment < 35 y/o Ceftriaxone 250 mg IM Doxycyxline 100 BID x 14 days > 50 y/o Treat responsible organism Ciprofloxin/Quinilones TMP/SMZ Orchitis DEFINITION: Inflammation or infection of the testicles may be related to epididymitis Extension to testes Etiology: bacterial (E. coli, K. pneumoniae, P. aeruginosa, Staph. or Strep) viral (EBV, coxsackievirus, arbovirus, enterovirus, MUMPS VIRUS) ORCHITIS & MUMPS Most common cause of orchitis Approximately 20% of prepubertal patients with mumps develop orchitis. 4 out of 5 cases occur in prepubertal males(younger than 10 years). Mumps orchitis follows the development of parotitis by 4-7 days. Mumps orchitis presents unilaterally in 70% of cases (fertility usually maintained) In 30% of cases, contralateral testicular involvement follows by 1-9 days. ORCHITIS SIGNS & SYMPTOMS: similar to epididymitis, hematuria, ejaculation of blood Pain, entire testes swollen- exquisitely tender Systemic- fever chills, malaise Orchitis - Treatment GENERAL: BED REST, SCROTAL SUPPORT ANALGESICS, ANTIEMETICs VIRAL etiology- Supportive care Orchitis- Treatment BACTERIAL etiology: <35 y/o and sexually active, antibiotic coverage for sexually transmitted pathogens (particularly gonorrhea and chlamydia) Ceftriaxone and either doxycycline or azithromycin is appropriate. >35 y/o with bacterial etiology require additional coverage for other gram-negative bacteria fluoroquinolone ( not for gonorrhea) TMP-SMX Section 3 PAINLESS SCROTAL MASSES PAIN LESS SCROTAL MASSES Varicocele Hydrocele Hernia Testicular Tumors Spermatocele Scrotal Edema Varicocele •Patient presents with mass of scrotum that feels like “bag of worms” •Most commonly left sided due to drainage of L gonadal vein into the left renal vein at an acute angle and anatomic variants which cause back pressure •Clinically benign Except in the setting of infertility •40% of men with infertility have varicocele. •Surgical removal may be necessary • Why might this cause infertility? Varicocele Hydrocele DEFINITION: Fluid filled mass between tunica vaginalis & testicle ETIOLOGY failure of patent processus vaginalis to close & failure of peritoneal fluid to be re-absorbed EPIDEMIOLOGY Common in newborns 1-6/100 boys Rarer in Adult males 1/100 When persistent or fluctuating Hydrocele seen after age of 1 a communication is present- (known as communicating Hydrocele) HYDROCELE RISK FACTORS Premature and low-birth-weight infants Indirect inguinal hernia Primary testicular/intrascrotal pathology Trauma Surgery Increased intra-abdominal pressure Lymphatic obstruction Ventriculoperitoneal shunt Peritoneal dialysis Ehlers-Danlos syndrome Non communicating forms may result from trauma, infection or neoplasm Hydrocele Physical Exam Transilluminating mass-waxes and wanes May associated with a indirect hernia Consider ultrasound due to possibility of neoplasm causing Hydrocele Management Expectant- watch and wait Surgical resection Hydrocele C COMMUNICATING NORMAL NON-COMMUNICATING HERNIA: DEFINITION: ETIOLOGY: EPIDEMIOLOGY: HERNIA:RISK FACTORS Being male. Family history. Certain medical conditions: cystic fibrosis Chronic cough.. Chronic constipation. Straining during bowel movements Excess weight: moderately to severely overweight puts extra pressure on abdomen. Pregnancy: This can both weaken the abdominal muscles and cause increased pressure inside your abdomen. Certain occupations: Having a job that requires standing for long periods or doing heavy physical labor increases risk of developing an inguinal hernia. Premature birth: Infants who are born early are more likely to have inguinal hernias. History of hernias: one inguinal hernia, it's much more likely develop another — usually on the opposite side. Hernias: EXAM Hernias Hernias Hernias Hernias CLINICAL COURSE: NORMAL: REDUCIBLE Complications: INCARCERATION Not easily manually reduced STRANGULATION Surgical Emergency- herniorrhaphy Blood supply to hernial contents (omentum/intestines) is compromised tissue death Spermatocele DEFINITION: Usually asymptomatic, small mass of the epididymis Benign DIAGNOSIS: Equivalent of a Berry aneurysm of the epididymis normally confirmed with ultrasound however only (definitive diagnosis is made through biopsy or aspiration returning spermatozoa- not necessary) TREATMENT: Surgical excision reserved for chronic pain or extensive enlargement CRYPTORCHIDISM DEFINITION: Undescended or“Hidden testis” EPIDEMIOLOGY: Incidence 0.7-1% at age 1. ETIOLOGY: Uncertain COMPLICATIONS: Can lead to infertility and has a higher incidence of malignancy . Tx- Orchiopexy TESTICULAR TUMORS EPIDEMIOLOGY: Incidence low: 4/100,000 Prevalence: 3.7/100,000 Most common cancer in men between ages of 15-35 Excellent prognosis with early detection Who gets testicular cancer? Men who are more likely to get testicular cancer: Are white Have a father or brother who had testicular cancer Have a testicle that did not come down into the scrotum even if surgery was done to remove the testicle or bring it down Have small testicles or testicles that aren't shaped right (most testicles are round, smooth and firm) Have Klinefelter's syndrome What are the signs of testicular cancer? A hard, painless lump in the testicle (this is the most common sign) Pain or a dull ache in the scrotum A scrotum that feels heavy or swollen Bigger or more tender breasts Back Pain Dyspnea Testicular Cancer Histology: 2 groups Nongerminal (5%) Leydig or sertoli cells GERMINAL (95%) Seminoma, Embryonal, tertatoma, choriocarcinoma, yolk sac tumors Testicular Cancer Germinal tumors usually metastasize thru lymph system except for choricocarcinoma which metastasize thru the vascular system. TREATMENT AND PROGNOSIS varies with type of tumor. The earlier its found the better the outcome! Virtually 100% CURE if found before metastasis >80% if metastasized chemotherapy Testicular Self Examination Check your testicles one at a time. Use one or both hands. Cup your scrotum with one hand to see if there is any change. Testicular Self Examination Place your index and middle fingers under a testicle with your thumb on top. Gently roll the testicle between your thumb and fingers. Feel for any lumps in or on the side of the testicle. Repeat with the other testicle. Testicular Self Examination Feel along the epididymis for swelling



![[2015.114] Sonographic Imaging of Scrotal Emergencies Including](http://s3.studylib.net/store/data/008082656_1-f1115c11919231e1b74639be8e0c7a09-300x300.png)