Nursing Daily Charting - N204 & N214L Psychiatric / Mental Health
Daily Charting 1
Nursing Daily Charting
Student:
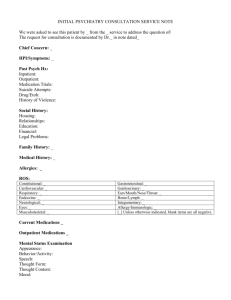
Client History
Name (initials only): Age:
Legal Status
(Vol, 5150, 5250, Conservatorship, T-Con):
Date of Admission:
Language:
Marital Status:
Education:
Ethnicity:
Occupation:
Psychiatric Diagnosis (Axis I):
Personality Disorder / Mental Retardation (Axis II):
Psychosocial and Environmental Problems (Axis IV):
(problems with primary support group, education, occupational, housing, economic, access to heath care)
Global Assessment of Functioning (Axis V):
Date:
Sex:
Presenting Problem
Reason for hospitalization (Client’s own words):
Current stressors:
Mental Status Examination
Appearance
(e.g. showered & groomed, wearing clean clothes, bizarre, inappropriate, disheveled, heavy make up)
:
Behavior & Motor Activity
(Calm, hyperactive, bizarre gestures, mannerisms, tics, tremors, psychomotor retardation, restlessness, repetitive behavior, other)
:
Daily Charting 2
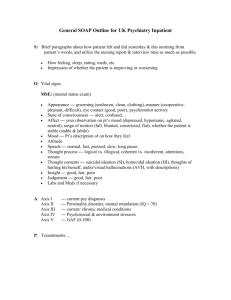
Attitude
(cooperative, uncooperative, friendly, hostile, guarded, suspicious, belligerent)
:
Affect
(blunted, flat, guarded, labile, expansive, sad, other)
:
Mood
(euthymic, angry, anxious, expansive, euphoric, irritable, apathetic, sad, other)
:
Speech
(normal rate, rhythm & tone, slowed, prolonged, speech latency, soft, loud, spontaneous, slurred, pressured, other)
:
Thought Content:
Suicide Ideation:
Homicidal Ideation:
Hallucinations
(auditory, visual, olfactory, gustatory, tactile)
:
Delusions
( bizarre, jealous, somatic, persecutory, paranoid, control, grandiose, religious, erotomania):
Thought Process
(logical, coherent, goal directed, illogical, circumstantial, tangential, flight of ideas, loose association, preservation, rumination, confabulations, confusion, other)
:
Cognition
(orientation, memory recall, concentration, attention span)
:
Insight: Judgment:
Coordination/gait/notable movement:
Cultural issues and religious affiliation that may affect his/her care:
Familial Concerns:
Current Health (Axis III)
Vital Signs T: P: R:
Pain (Numeric 1-10): Location: Character:
How would you describe your health: Excellent Average
Medical and (or) physical problems:
BP:
Good Poor
Nutritional Status: Diet: Feeding supplement:
Chewing difficulty:
Elimination Pattern:
Activity-Exercise Pattern:
Sleep-Rest Pattern:
Substance Abuse:
Substance Amount / Frequency Duration
Signs of withdrawal symptoms:
Teaching assessment:
Discharge Plans:
Additional data:
Daily Charting 3
Swallowing difficulty:
Last Used
Daily Charting 4
Nursing Process
2.
3.
4.
Based on the nursing assessment you have just completed, Identify subjective and objective data and list all nursing problems including cultural issues and teaching needs (Prioritize Problems):
1.
Nursing Diagnosis (Actual or Potential):
Outcomes / Planning (measurable):
Interventions:
Evaluation (patient response to interventions):