Metabolic Response to Trauma
advertisement

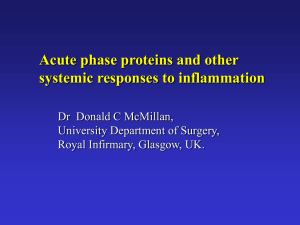
METABOLIC RESPONSE TO TRAUMA Dr. Dalal AL-Matrouk Introduction • Following accidental or deliberate injury, a characteristic series of changes occurs, both locally at the site of injury and within the body generally. • These changes are intended to restore the body to its pre- injury condition. Introduction • Many of these physiological changes can be modified or corrected by treatments. • Although the metabolic response aims to return an individual to health, it can sometimes have harmful effects. For example, a major response can damage organs distant to the injured site itself. Phases of the metabolic response to trauma Two phases: the ‘ebb’ and the ‘flow’ Ebb: - usually comprised the first few hours after injury - cold and hypotensive 1. 2. flow: - initial catabolic phase high metabolic rate, breakdown of proteins and fats, a net loss of body nitrogen and weight loss. - followed by an anabolic phase protein and fat stores were restored and weight gain 5 Ebb or shock phase • Immediately following injury • Usually brief in duration; 12 to 24 hours • Reduced: Blood pressure, cardiac output, body temperature and oxygen consumption • Often associated with hemorrhage, resulted in hypoperfusion and lactic acidosis 6 Flow phase • Hypermetabolism • increase in basal metabolic rate • increased oxygen consumption & cardiac output • increased urinary nitrogen losses, altered glucose metabolism, accelerated tissue catabolism 7 Altered glucose metabolism • Hyperglycemia • Ebb phase • parallel severity of stress • low insulin levels • glucose production only slightly elevated • Flow phase: • hyperglycemia persist • insulin levels-normal or elevated • increase hepatic glucose production • profound insulin resistance FACTORS MEDIATING THE METABOLIC RESPONSE TO INJURY • The metabolic response is a complex interaction between many body systems. Injury response Neurohormonal + Inflammatory THE ACUTE INFLAMMATORY RESPONSE • Physical damage to tissues results in local activation of cells such as tissue macrophages. • These cells release a variety of cytokines. SOME CYTOKINES INVOLVED IN THE ACUTE INFLAMMATORY RESPONSE • TNF-a • IL-1 • IL-8 • IL-6 • IL-10 THE ACUTE INFLAMMATORY RESPONSE • The effects of the inflammatory response mediators can be localized (paracrine effect) or become generalized in the body (endocrine effect). • This cascade of events results in rapid amplification of the initial stimulus large numbers of inflammatory cells at the injured site mediating the inflammatory response via cytokines. THE ACUTE INFLAMMATORY RESPONSE • Other pro-inflammatory substances are released in association with tissue injury. • These include prostaglandins, kinins, complement and free radicals. • Anti-inflammatory substances and mechanisms also exist, such as antioxidants (e.g. glutathione, vitamin A and vitamin C) and protease enzyme inhibitors (e.g. a2macroglobulin) 15 Acute phase proteins • Fibrinogen • C-reactive protein • Inhibit generalized tissue destruction from inflammation 16 Neurohormonal response Neuro Response Stimulation of the sympathetic nervous system: • results in tachycardia and increased cardiac output. • Noradrenaline release from sympathetic nerve endings and adrenaline release from the adrenal gland increase circulating catecholamine concentrations. ENDOCRINE RESPONSE • Hormonal changes are mainly involved in maintaining the body’s fluid balance and in the changes to substrate metabolism that occur following injury. Consequences of metabolic response to injury Hypovolemia: Due to fluid loss/sequestration neuroendocrine response to restore normal fluid status Fluid conserving measures: - ADH: promotes water retention - Aldosterone: reabsorbtion of sodium & excretion of potassium & hydrogen - Duration of high ADH & Aldosterone:48-72 hrs Blood conserving measures: Hypovolemia low C.O decreased blood flow to organs neuroendocrine response to increase C.O (SV X HR) Consequences of metabolic response to injury INCREASED ENERGY METABOLISM : • Following severe trauma, resting energy expenditure is increased by 50%. • Thermogenesis: metabolic rate is increased by 6- 10% for each 1C increase in T • Catabolism is mediated by catecholamines & cytokines changes in carbohydrate, protein & fat metabolism Consequences of metabolic response to injury Changes in RBC synthesis & coagulation: 1. Anemia : - bleeding - hemodilution - impaired BM function (less erythropoitin) - changes in iron metabolism (less available iron) 2. Hypercoagulability: - Activation of plts by epinephrine & cytokines - Dehydration & immobility - Increased procoagulants (fibrinogen) & decreased anticoagulants (protein C) Consequences of metabolic response to injury Changes in RBC synthesis & coagulation: 3.Hypercoagulability: - Rare - Assocaited with shock, massive blood transfusion or sepsis - Exteme form: DIC Factors modifying the metabolic response to injury • Patient-Related factors: - Genetic predisposition - Coexisting disease - Drug treatments - Nutritional status Factors modifying the metabolic response to injury • Surgical/trauma-Related factors: - Severity of injury - Nature of injury ( e.g burn) - Ischemia-reperfusion injury - Tempreture/infection - Anesthetic technique TO SUMMARIZE THANK YOU