Acute phase proteins and other systemic responses to inflammation
advertisement

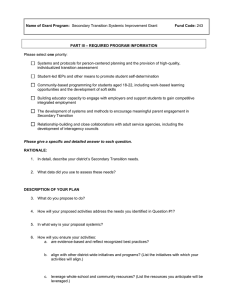
Acute phase proteins and other systemic responses to inflammation Dr Donald C McMillan, University Department of Surgery, Royal Infirmary, Glasgow, UK. Shock/ hypoxia Infection SYSTEMIC INFLAMMATION Pancreatitis MODS Trauma Infective diseases Burn Non-infective diseases Ebb and flow phases of Cuthbertson Ebb Flow Phase Pre-resuscitation phase Poor tissue perfusion Hypometabolic Decreased energy expenditure Increased glucocorticoids Increased catecholamines Low insulin Normal glucose production Mild protein breakdown Recovery phase Normal tissue perfusion Hypermetabolic Increased energy expenditure Normal glucocorticoids Normal catecholamines Increased insulin Increased glucose production Profound protein breakdown The metabolic response to injury Cuthbertson et al. 1930 Pathophysiological changes of the systemic inflammatory response Neuroendocrine changes Fever, somnolence, fatigue and anorexia Increased adrenal secretion of cortisol, adrenaline and glucagon Haematopoietic changes Anaemia Leucocytosis Thrombocytosis Metabolic changes Loss of muscle and negative nitrogen balance Increased Lipolysis Trace metal sequestration Diuresis Hepatic changes Increased blood flow Increased acute phase protein production Gabay and Kushner, NEJM, 1999 Mediators of the metabolic response to injury Cuthberston (1930) Increased protein breakdown and REE Selye (1940’s) Corticosteroids proposed as mediator Allison (1960’s) Insulin resistance proposed as mediator Cytokines (1980’s) TNF, Il-1, Il-6 proposed as mediators Adipokines (1990’s) Leptin, adiponectin, ghrelin? Mediators of the metabolic response to injury Hormonal Metabolic Chemical Catecholamines REE pH Glucagon Hyperglycemia Prostanoids Corticosterioids Ketoacidosis Leukotrienes Insulin Resistance Uremia Cytokines SIRS (Systemic Inflammatory Response Syndrome) • The systemic response to a wide range of stresses. – Temperature >38°C (100.4°) or <36°C (96.8°F). – Heart rate >90 beats/min. – Respiratory rate >20 breaths/min or PaCO2 <32 mmHg. – White blood cells > 12,000 cells/ml or < 4,000 cells/ml or >10% immature (band) forms. • Note – Two or more of the following must be present. – These changes should be represent acute alterations from baseline in the absence of other known cause for the abnormalities. American College of Chest Physicians/Society of Critical Care Medicine Consensus. Crit Care Med. 1992;20:864-874. Acute phase proteins and the systemic inflammatory response Gabay and Kushner, 1999 C-reactive protein in patients undergoing curative surgery for colorectal cancer Crozier et al., 2004 Resting energy expenditure in injury Skeletal Trauma Major Burn Multitrauma Closed Head Injury Sepsis Elective Surgery Starvation -20 0 20 40 % Above Usual Requirement 60 80 Resting energy expenditure in disease Cancer Acute Renal Acute Renal Liver Failure Lung (COPD) GI (Crohn's) -40 -20 0 20 % Above Usual Requirement 40 60 Energy Requirements Following Surgery Resting energy expenditure increased by 10-50% to support increased metabolic workload An additional allowance is added for activity 20 % if confined to bed 30 % if ambulatory Surgery: Protein & Amino Acid Metabolism If there are insufficient protein reserves there is: decreased wound healing decreased immune response defective gut-mucosal barrier decreased mobility/ respiratory effort Loss of Lean Body Mass Lean body mass= body cell mass metabolically active compartment Irreversible at some point critical mass Protein requirements are increased to accommodate: • • • • Immune response Increased metabolic activity Replacement of damaged cells Replacement of protein losses – perspiration, blood, exudates, renal, intestinal – if anorexia accompanies fever/infection – by muscle proteolysis Operative measures to reduce protein loss in surgical injury Minimise the inflammatory stimulus Surgical techniques Anaesthesia Control of sepsis Environmental temperature Control of pain and anxiety Nutritional intervention If oral intake less than 60% of energy and protein requirements by 10 days Injury and the systemic inflammatory response Activation of white blood cells, fibroblasts, endothelial cells CIRCULATION C-reactive protein Albumin Haemoglobin Zinc Iron Copper Retinol Alpha-tocopherol Carotenoids WHOLE BODY Resting energy expenditure Weight loss QUALITY OF LIFE Fatigue Performance status HEALING Body cell Mass INFLAMMATORY PROCESS Release of Il-6, Il-1, TNF, Interferons, growth factors Conclusions The systemic inflammatory response plays an important role in determining protein loss in acute and chronic disease. Acute phase proteins in particular C-reactive protein and albumin are useful in quantifying the magnitude of this response and both are associated with poor outcome