Warts and All
Dr Daniela Brawley
ST4
Genitourinary medicine
23rd November 2010
Cases of genital warts/year in UK
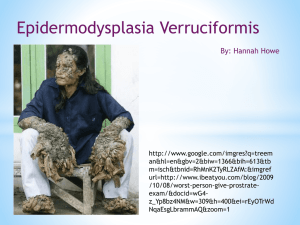
Human Papilloma Virus
> 100 sub-types of HPV
HPV 6 and 11 cause 90% of genital warts
Most clear the infection in 9 months
HPV 16 and 18 risk for malignant change
–
Persistent infection with oncogenic sub-types
increases risk of malignant change
Prevalence
1% of population have visible warts
10% have active HPV infection
60% have cleared HPV
–
However can have long latent or lifelong phase
? Missed opportunity with quadrivalent HPV
vaccine (6/11/16/18)
Transmission
Sexual in majority of cases
–
–
Female to male 71% at 3 months
Male to female 54% at 3 months
Condoms can reduce risk but don’t eliminate
Increased risk if immunocompromised and/or
smoker
Diagnosis
Diagnosis is by examination under good light
Consider referral/biopsy if atypical or unsure
STI screening
Partner notification not necessary
STI screening
10-20% have co-existing STIs
Extensive warts – HIV indicator disease
–
Chlamydia/ Gonorrhoea
–
–
BHIVA 2008 HIV testing guidelines
Urine in males
Vulvovaginal/cervical swab in females
HIV/Syphilis
But first…
….what’s a normal lump?
Pearly penile papules
Normal anatomy
No treatment
Common presentation in young men
Reassure strongly that are normal
Vulval papillomatosis
Smooth and symmetrical
Easily confused with HPV
Don’t progress
–
review at 1 month
No treatment
Parafrenular glands
Symmetrical, small and smooth surface
No treatment required
Fordyce spots or sebaceous follicles
Glands in clusters
Prepuce, shaft of penis and vestibular area
of vulva
More obvious when skin is stretched
Reassurance
Sebaceous cysts
No treatment necessary unless become too
large or get infected
Reassurance
In men scrotal sebaceous cysts may occur
Lymphocoele
Hard swelling behind coronal surface
No treatment required
Usually resolves over time
Reassurance
And now…
other differentials
Molluscum contagiosum
Pox virus
Skin to skin contact, most likely sexual
Cryotherapy
STI screening including HIV especially if
extensive
Condyloma Lata of Secondary Syphilis
Refer GUM
Syphilis PCR and serology
Dark ground microscopy
STI screening
Penicillin and GUM follow-up
Now for warts….
Site, distribution and number
Morphology- keratinised or non keratinised
Patient features
Experience and equipment
–
Availability of cryotherapy
Treatments
Podophyllotoxin (warticon)
Cryotherapy
Imiquimod (aldara)
Smoking cessation
Excision
Warticon
Purified extract of podophyllin
Solution (0.5%) or cream (0.15%)
Non-keratinised warts, not perianal
3 days BD then 4 days rest for 4 weeks
Soreness and ulceration
NOT used in pregnancy
Cryotherapy
Necrosis of dermal-epidermal junction
Keratinised warts and intrameatal warts
Weekly application with “Halo” and “Freeze
and thaw” techniques
Safe in pregnancy
Aldara
Immune response modulator
Non formulary and expensive (£50/month)
Used for resistant/extensive warts
3 times a week for maximum 16 weeks
NOT used in pregnancy
Source: Sandyford ProtocolsExternal Anogenital Warts.
Clearance rates
TREATMENT
END OF
TREATMENT
>3 MONTHS
RECURRENCE
RATES (%)
Cryotherapy
63-88 (75)
63-92
0-39 (20)
Imiquimod
(Aldara)
50-62 (58)
50-62
13-19 (16)
Podophyllotoxin
(Warticon)
42-88 (65)
34-77
10-91 (50)
Surgical excision
89-93 (91)
36
0-29 (15)
Source: United Kingdom National Guideline on the Management of Anogenital
Warts, 2007. (BASHH)
Keratinised Warts
Cryotherapy first line
Imiquimod if not improving
Warticon less likely to be effective but can try
for 4 weeks
Non-keratinised warts
Warticon
Cryotherapy or imiquimod if not improving
Perianal warts
Cryotherapy first line
Imiquimod if not improving
Warticon can be used but not licensed
Proctoscopy not indicated unless immune
suppressed, or symptoms in anal canal
Extensive Sub-preputial warts
GUM referral
Imiquimod and cryotherapy
Surgical referral
20 week pregnant female
Warts in pregnancy
Cryotherapy
Warticon and Imiquimod contraindicated
Improve/resolve 6-8 weeks after delivery
Not an indication for Caesarean Section
Small risk of transmission both genital and
laryngeal papilloma
–
–
1 in 400
No reduction with c-section
Warts and Bowen’s Disease
Referral for biopsy of suspicious areas
Cryotherapy/ electrocautery
Circumcision
Warts and VIN
Referral for biopsy of suspicious areas
Localised surgical excision
Referral to Gynaecology
Features indicating biopsy
Atypical
Pigmentation
Flat warts
Older age groups
Immunosuppression including HIV
Heavy smokers
Extensive warts
Trial of imiquimod +/- cyrotherapy
Referral to Gynaecologist for surgical
removal
STI screening
Single wart at fourchette
Cryotherapy
Surgical excision
Extensive anal warts HIV positive gay
man
GUM referral
Syphilis PCR and serology
Cryotherapy and/or Imiquimod
Proctoscopy
Surgical referral
–
Risk of AIN
Meatal Warts
Cryotherapy
–
If can see extent of warts
Concern about causing urethral stenosis
Warn about symptoms of urethral
obstruction
Vaginal warts
Usually resolve with treatment of external
warts
Cryotherapy if not improving
Cervical warts
Usually resolve with treatment of external
warts
Ensure has had recent smear
–
No need for additional smears
If no external warts or no improvement with
treatment of external warts refer to
colposcopy
Summary points
Treat the patient in front of you
Offer STI testing
Smoking cessation
Refer if unsure, not improving or suspicious
features
Sandyford contacts
www.sandyford.org
0141 211 8130
dbrawley@nhs.net
Some final points…
Chlamydia/Gonorrhoea NAAT test
PREFERRED SAMPLE
VULVOVAGINAL SWAB
Tests for ulcers
Syphilis
Herpes type 1 and 2
Combined PCR test
Confirm with
syphilis serology
PRIMARY CARE VAGINAL DISCHARGE PROTOCOL
History
Low risk STI
Typical BV or VVC history
No symptoms of PID
High risk STI
Pregnant
Requests testing
Examination and pH
Examination, pH and
CT/GC NAAT
Exam
HVS
CT/GC NAAT
CT/GC NAAT
pH < 4.5
Treat for
VVC
pH > 4.5
Treat for BV
pH < 4.5
Treat for VVC
Await CT/GC
NAAT
Recurrence
Symptoms of PID
Postpartum
Gynaecological instrumentation
pH > 4.5
Treat for BV
Await CT/GC
NAAT
GUM referral if GC positive
or unresolved
BV- bacterial vaginosis
VVC- vulvovaginal candida
CT/GC NAAT- Chlamydia/Gonorrhoea molecular te
GUM- genitourinary medicine clinic