Verrucae, current treatment regimes
advertisement
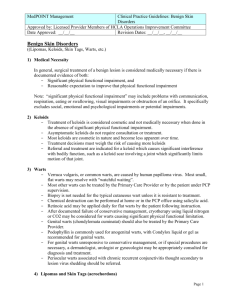
VERRUCAE, CURRENT TREATMENT REGIMES KERWIN TALBOT OUTLINE • BIOLOGY OF WARTS • EPIDEMIOLOGY • DIFFERENTIAL DIAGNOSIS • TREATMENT FACTORS • TREATMENTS BRIEF SUMMARY OF THE LARGE VARIETY OF TREATMENTS IN-DEPTH EXAMINATION OF THE HIGHER EVIDENCE BASED TREATMENTS • DISCUSSION • CONCLUSION BIOLOGY OF WARTS • CUTANEOUS VIRAL WARTS, CAUSED BY THE HUMAN PAPILLOMA VIRUS • (HPV) • DNA VIRUSES, WHICH INFECT EPITHELIAL CELLS • MINOR ABRASIONS AND INFECTIONS FREQUENTLY SERVE AS CONDUITS FOR HPV • REMAIN DORMANT WITHOUT VISIBLE DISEASE • THE MOST COMMON INFECTIONS ARE WITH HPV TYPE 1,2, 4, 37 AND 57 ON THE HANDS AND FEET. EPIDEMIOLOGY OVERALL PREVALENCE OF WARTS OF 32.8/1000 IN THE 15 TO 74 YEARS AGE RANGE. • YOUNGER GENERATION- HIGHER PREVALENCE VIRAL ACTIVITY LIKELY DEPENDS ON: • IMMUNE STATUS • RESPONSE OF THE INFECTED INDIVIDUAL SEROCONVERSION AFTER NATURAL INFECTION IS : • RELATIVELY SLOW • VIRAL LOAD • PERSISTENT INFECTION • RECURRENCE AFTER CLINICAL CURE IS OFTEN DUE TO LATENT VIRUS VERSUS REINFECTION DIFFERENTIAL DIAGNOSIS WARTS ARE IDENTIFIED BY: A CHANGE IN THE REGULAR PAPILLARY SKIN LINES WITH INDEPENDENT VASCULAR SOURCES. HPV CAN MASQUERADE AS: • A SEBORRHEIC KERATOSIS, • CALLUS, • CORN, • EPIDERMAL NEVUS, • MOLLUSCUM CONTAGIOSUM OR SQUAMOUS CELL CARCINOMA. IS IT IMPORTANT TO KEEP THESE IN MIND- IF UNSURE HISTOLOGICAL EXAMINATION MAY NEED TO BE PERFORMED. INDICATIONS FOR WART TREATMENT • DEVELOPED BY THE AMERCIAN ACADEMY OF DERMATOLOGY 1) THE PATIENT’S DESIRE FOR THERAPY, 2) SYMPTOMS OF PAIN, BLEEDING, ITCHING OR BURNING, 3) DISABLING OR DISFIGURING LESIONS, 4) LARGE NUMBERS OR LARGE SIZES OF LESIONS, 5) THE PATIENT’S DESIRE TO PREVENT THE SPREAD OF WARTS TO UNBLEMISHED SKIN OF SELF OR OTHERS, AND 6) AN IMMUNOCOMPROMISED CONDITION. TREATMENT FACTORS WHEN CHOOSING A TREATMENT • AGE • SITE OF INFECTION, • SIZE, • NUMBER AND TYPES, • IMMUNOLOGICAL STATUS, • TREATMENT AVAILABILITY, • COST, • PATIENT’S DESIRE FOR THERAPY, • ABILITY TO ADHERE, • PAIN TOLERANCE. SUMMARY OF TREATMENTS Treatment categories Treatment Folk and alternative treatments • Folklore • Hypnosis/Suggestive Therapy • Garlic Extracts • Duct Tape Destructive therapy • Surgical Removal by Curettage or Cautery • Salicylic Acid • Cantharidin • Cryotherapy • • • • • • • • Exothermic Patches Ultrasound Hyperthermia Radiofrequency Ablation Microwave Treatment Infrared Coagulation Carbon Dioxide (CO2) Laser Pulsed Dye Laser Photodynamic Therapy SUMMARY OF TREATMENTS Treatment categories Treatments Virucidal Therapy • Glutaraldehyde • Formaldehyde • Formic Acid • Antiviral Drugs Antimitotic Therapy • • • • Immunotherapy • Oral Zinc Sulphate Bleomycin Retinoids Podophyllin Podophyllotoxin • Contact Sensitizers • Intralesional Injection of Interferon • 5-Fluorouracil (5-FU) Combination Therapies • 5-FU + Salicylic Acid • Cryotherapy + Podophyllotoxin • SA + cryotherapy TREATMENT SPECIFICS Treatment type Treatment Cost Reported efficacy Reported pain Reoccurrence Side effects Alternative remedies Destructive Duct tape Low High* 85% Low Not reported None (allergy) Surgical High* Low High -30% Scarring Silver nitrate Low* High* 6585% Mod 43% Low* Mod 15% Salicylic acid Low* Mod-high 70% Low -mod Low Clinical burns Irreversible tissue staining Localised burns Contact dermatitis Cryotherapy Traditional Mod* Low-mod 30% Mod Low Aggressive Mod* Mod 50% Mod-high* Low Virucidal therapy Formalin Low* (aqueous solution) Immunothera Oral zinc sulphate Low* py Combination Salicylic acid and Mod* therapies cryotherapy Blistering and pain* (44%) Mod-high 60-67% Low Low Increase risk and severity (64%) Sensitivity* High 87% Low Not reported Minimal High 50100% Mod-high Low Clinical burns Blistering Pain TREATMENTS KEY RECOMMENDATIONS FOR PRACTICE Clinical recommendation Evidence rating Topical salicylic acid therapy is recommended A Cryotherapy is not recommended over salicylic acid for treatment Aggressive is recommended over traditional A Surgical is only recommended over salicylic acid in case by case basis B Sliver nitrate is recommend for patients with low pain tolerance and children and facial areas B Formalin has found to be effective, pain less and have minimal side effects B/C There is poor evidence to recommend pulsed dye laser therapy B TREATMENTS SALICYLIC ACID (SA) • KERATOLYTIC THERAPY • OVER-THE-COUNTER- 17% SALICYLIC ACID • THERAPEUTIC- UP TO 80% SOLUTION. ADVANTAGES: • CONVENIENCE, MINIMAL EXPENSE, NEGLIGIBLE PAIN AND REASONABLE EFFECTIVENESS. DISADVANTAGES: • REQUIRE WEEKS TO MONTHS OF TREATMENT, AND THE PATIENT COMPLIANCE RECOMMENDED METHOD: • HIGHER CONCENTRATION – BETTER RESULTS WITH 60%, • OCCLUSIVE DRESSING, • OFF-LOADING PADDING MINIMISED PAIN IN WEIGHT BEARING AREAS • 1 WEEK WITH TREATMENT ON, TREAT EVERY 2 WEEKS – BEST RESULTS SA THERAPY SHOULD REMAIN AS THE RECOMMENDED FIRST-LINE THERAPY TREATMENTS CRYOTHERAPY • AGGRESSIVE CRYOTHERAPY TO BE SIGNIFICANTLY MORE EFFECTIVE THAN GENTLE/TRADITIONAL. • CRYOTHERAPY TECHNIQUES CAN VARY • APPLICATION MODE, - NO DIFFERENCE BETWEEN PEN OR SPRAY • FREEZE TIMES- AGGRESSIVE OVER TRADITIONAL/ GENTLE • INTERVALS BETWEEN TREATMENTS- EVERY 2 WEEKS • DEBRIDEMENT IMPORTANT ADVANTAGES: EFFECTIVE, EASY, ACCESSIBLE (OVER COUNTER) DISADVANTAGES: HYPOPIGMENTATION/ HYPERPIGMENTATION, INFECTION RISK, VASCULAR STATUS CRYOTHERAPY, RECOMMENDED AS A SECOND-LINE THERAPY OR AS A COMBINATION TREATMENT. TREATMENTS SILVER NITRATE CAUTERIZING AGENT TO REMOVE TISSUE AND BLOOD VESSELS. ANTIMICROBIAL ACTIVITY METHOD RECOMMENDED FOR 10% - EVERY OTHER DAY FOR APPROXIMATELY 1-2 MINUTES FOR THREE WEEKS WITH HEAVY DEBRIDEMENT AS THE CONCENTRATION INCREASES 25%, 50% AND 75% THE DURATION BETWEEN APPLICATION CAN INCREASE AND LENGTH OF ADMINISTRATION SHORTEN. INCREASED RISKS OF SIDE EFFECTS WITH INCREASED CONCENTRATIONS. TREATMENTS POTASSIUM HYDROXIDE POWERFUL CAUSTIC AGENT KERATOLYTIC AGENT – MULTIPLE DERMATOLOGICAL USES METHOD RECOMMENDED: 5% : ONCE NIGHTLY, FOR 4 WEEKS, WEEKLY HEAVY DEBRIDEMENT. SIDE EFFECTS: ITCHING, BURNING SENSATION, ERYTHEMA AND TEMPORARY DYSPIGMENTATIONS. 5% HAD A 77.6% CURE RATE AFTER 4 WEEKS 10% HAD A 88.9% CURE RATE AFTER 4 WEEKS RECOMMENDED TO AVOID EYE CONTACT TREATMENTS FORMALIN DISRUPTING THE UPPER LAYERS OF THE EPITHELIAL CELLS KILLING THE VIRIONS METHOD RECOMMENDED: DEBRIDEMENT, DAILY APPLICATION, FILING BEFORE APPLICATION, OCCLUDE WITH DRESSING. SOAKS HAVE A HIGHER CURE RATE BUT ALSO INCREASED REPORTED SENSITIVITY. RECOMMEND NOT TO INHALE SOLUTION / MASK DURING APPLICATION AS A PRECAUTION. MINIMAL SIDE EFFECTS, COST AND PAIN MODERATE TO HIGH REPORTED CURE RATES – EVIDENCE IS OLD. TREATMENTS USING A TECHNIQUE OF MULTIPLE WART PUNCTURES WITH A BIFURCATED NEEDLE • IN STUDIES USED WITH ANOTHER TREATMENT, • FOUND A HIGHER CLEARANCE RATE USING THIS TECHNIQUE, • USED IN CONJUNCTION WITH LA / ANKLE BLOCK, • CAUSES AN INFLAMMATORY RESPONSE – EVOKES AN IMMUNE RESPONSE. TREATMENTS • THIRD LINE TREATMENTS: • BLEOMYCIN: • ADVANTAGES: • RESERVED FOR RECALCITRANT WARTS, • DNA AND PROTEIN SYNTHESIS ARE INHIBITED, AND APOPTOSIS IS TRIGGERED. • DISADVANTAGES: • SIGNIFICANT SYSTEMIC DRUG EXPOSURE • EXPENSIVE AND PAINFUL • RAYNAUD’S PHENOMENON DISCUSSION • ENORMOUS VARIETY OF WART TREATMENT, • CHOOSING THE BEST WART TREATMENT, • OVER 6 MONTHS- RECALCITRANT • REMISSION AND RECURRENCE • INVASIVE METHODS - PAINFUL AND REQUIRE LONG RECOVERY TOPICAL MANAGEMENT- DEPENDENT ON: • PATIENT COMPLIANCE • LONG APPLICATION PERIODS CONCLUSION • EVIDENCE TO SUPPORT THE USE OF SA • CRYOTHERAPY- SECOND-LINE THERAPY/ ALTERNATIVE TREATMENT • THIRD-LINE TREATMENTS • TAILORED • MORE HIGH-QUALITY EVIDENCE REFERENCES • GIBBS S, HARVEY I, STERLING J ET AL. LOCAL TREATMENT FOR CUTANEOUS WARTS: SYSTEMATIC REVIEW. BMJ 2002; 325:461–4. • GIBBS S, HARVEY I. TOPICAL TREATMENTS FOR CUTANEOUS WARTS. COCHRANE DATABASE SYST REV 2006; 3:CD001781. • BACELIERI R, JOHNSON SM. CUTANEOUS WARTS: AN EVIDENCE-BASED APPROACH TO THERAPY. AM FAM PHYSICIAN 2005; 72:647–52. • WILLIAMS HC, POTTIER A, STRACHAN D. THE DESCRIPTIVE EPIDEMIOLOGY OF WARTS IN BRITISH SCHOOLCHILDREN. BR J DERMATOL 1993; 128:504–11. • 3 REA JN, NEWHOUSE ML, HALIL T. SKIN DISEASE IN LAMBETH. A COMMUNITY STUDY OF PREVALENCE AND USE OF MEDICAL CARE. BR J PREV SOC • MED 1976; 30:107–14. • 4 MASSING AM, EPSTEIN WL. NATURAL HISTORY OF WARTS. ARCH DERMATOL 1963; 87:306–10. • LEMAN JA, BENTON EC. VERRUCAS. GUIDELINES FOR MANAGEMENT. AM J CLIN DERMATOL 2000;1:143-149. • DRAKE LA, CEILLEY RI, CORNELISON RL, DOBES WL, DORNER W, GOLTZ RW, LEWIS CW, SALASCHE SJ, TURNER ML, LOWERY BJ, • SHAMA SK, ANDROPHY EJ, GALEN WK, HEATON CL, LYNCH PJ,CHANCO TURNER ML. GUIDELINES OF CARE FOR WARTS: HUMAN • PAPILLOMAVIRUS. COMMITTEE ON GUIDELINES OF CARE. J AM ACAD DERMATOL 1995;32:98-103. • 26. MICALI G, DALL’OGLIO F, NASCA MR, TEDESCHI A. MANAGEMENT OF CUTANEOUS WARTS: AN EVIDENCE-BASED APPROACH. AM J CLIN • DERMATOL 2004;5:311-317. • BORORVOY MA, BOROVOY M, ELSON LM, SAGE M. FLASHLAMP PULSED DYE LASER (585 NM) TREATMENT OF RESISTANT VERRUCAE. JOURNAL OF THE AMERICAN PODIATRICMEDICAL ASSOCIATION 1996;86:547–50. • ALLENBY CF. THE TREATMENT OF VIRAL WARTS WITH GLUTARALDEHYDE. BRITISH JOURNAL OF CLINICAL PRACTICE 1977;31:12–3. • AMER M, DIAB N, RAMADAN A, GALAL A, SALEM A. THERAPEUTIC EVALUATION FOR INTRALESIONAL INJECTION OF BLEOMYCIN SULFATE IN 143 RESISTANT WARTS. JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY 1988;18(6):1313–6. • EL-TONSY MH, ANBAR TA, EL-DOMYATI M, BARAKAT M. DENSITY OF VIRAL PARTICLES IN PRE AND POST ND:YAG LASER HYPERTHERMIA THERAPYAND CRYOTHERAPY IN PLANTAR WARTS. INTERNATIONAL JOURNAL OFDERMATOLOGY 1999;38:393–8. • AL-GURAIRI FT, AL-WAIZ M, SHARQUIE KE. ORAL ZINC SULPHATE IN THE TREATMENT OF RECALCITRANT VIRAL WARTS: RANDOMIZED PLACEBO-CONTROLLED CLINICAL TRIAL. BR J DERMATOL 2002;146:423-431.