Responsibilities of Investigators
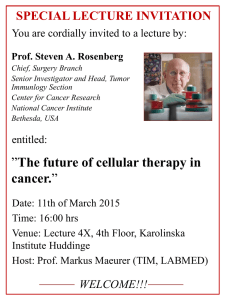
advertisement

GCP FOR INVESTIGATORS Tina Lidén Mascher, Kvalitetsregister, forskning och industrisamarbeten AGENDA Background Guidelines Informed consent procedures Investigator responsibilities- GCP, protocol Adverse Events Qualification, Training, equipment Study drugs- handling, storage, accountability Source data, Data collection Archiving GCP & Regulatory Compliance deficiencies BACKGROUND Good Clinical Practice (GCP) is a set of internationally recognised ethical and scientific quality requirements for designing, conducting, recording, and reporting Clinical Trials. Compliance with GCP provides assurance that the rights, safety and well-being of subjects are protected, while maintaining data quality throughout the study. The objective of this ICH GCP Guideline is to provide a unified standard for the EU, Japan, and the United States to facilitate the mutual acceptance of clinical data by the regulatory authorities in these jurisdictions. GUIDELINES The principles of GCP are defined in: ICH Guideline for Good Clinical Practice E6 (Guidance for Industry E6 Good Clinical Practice: Consolidated Guidance) adopted within Europe in July 1996 adopted within Japan in March 1997 adopted within the US in May 1997 INFORMED CONSENT Freely given informed consent should be obtained from every subject prior to clinical trial participation. Before informed consent may be obtained, the investigator or designee should provide the subject enough time and opportunity to inquire about details and to decide whether or not to participate in the trial. Prior to a subject’s participation in the trial, the informed consent form (ICF) should be signed and personally dated by the subject and by the person who conducted the informed consent discussion. A copy of the ICF should be provided to the subject. Before any trial procedure such as examinations/ evaluations and tests, it should be reconfirmed that the (ICF) has been obtained. ICF signature procedure must be always documented in the patients’ medical records. RESPONSIBILITIES OF INVESTIGATORS (1) The investigator should be qualified by education, training and experience to assume responsibility for the proper conduct of the trial, and should provide evidence of such qualifications through an up-to-date CV including GCP training/ experience. The investigator should be aware of, and should comply with, GCP and the applicable regulatory requirements. http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E 6_R1/Step4/E6_R1__Guideline.pdf Declaration of Helsinki: http://www.wma.net/en/30publications/10policies/b3/ To conduct study in full accordance with the current protocol. Trial provided materials such as check lists and flowcharts are useful tools to help with trial planning. To document and report any protocol deviations to the Company/Sponsor. RESPONSIBILITIES OF INVESTIGATORS (2) To report all AEs to Company. If a patient suffers an AE during an assessment the assessor shall report this to the Principal Investigator and ensure that it is documented and reported. Report any SAEs within 24 hours of becoming aware of the event to Company and IEC/Ethics committee and Health Authorities as applicable . To read and understand the Investigator’s Brochure (including potential risks and side effects of the IMP). To ensure that all study personnel are informed about their obligations and study duties. To maintain properly completed and accurate study records and to make those records available for monitoring, audits and inspection. Permit trial-related monitoring, audits, IEC review, and regulatory inspection(s), providing direct access to source data/ documents. RESPONSIBILITIES OF INVESTIGATORS (3) The investigator should maintain a list of appropriately qualified persons to whom the investigator has delegated trial-related duties. The Principal Investigator is responsible for ensuring that all trial staff is adequately trained on trial processes and procedures, as well as on the standardized working instructions used. Duties can be delegated, not responsibility. CRA should be always informed about all changes in study staff, study facilities and duties assignation as soon as they happen. For all equipment used by the site and departments, devices must be identified, calibrated and have documentation of controls. RESPONSIBILITIES OF INVESTIGATORS (4) All product accountability. Storage of the investigational product and ensure that all equipment (infusion pumps, freezers, refrigerator) used in the trial is adequately calibrated and controlled. The investigator or designee should maintain records of: • the product’s delivery to the trial site • the inventory at the site • study medication administered to each subject • destruction of unused product • destruction of used study medication (vials) DATA COLLECTION (1) Clinical Trial data must be recorded, handled and stored to enable accurate reporting, interpretation and verification. All trial data must be recorded in the paper/electronic Case Report Forms (CRFs) in a timely manner, preferably as soon as they are generated. The investigator should ensure the accuracy, completeness, legibility, and timeliness of the data reported to the sponsor in the CRFs and in all required reports (As per Section 4.9.1 of ICH E6) Data reported on the CRF, that are derived from source documents, should be consistent with the source documents or the discrepancies should be explained (As per Section 4.9.2 of ICH E6 Source documents can be hospital records, Lab reports, ECGs, MRIs, Patient Diaries, pharmacy records, etc. An explanation for the omission of any required data must be recorded on the appropriate page. Any data, CRF and information sheet collected should be signed and dated. Only the Principal Investigator or authorised Sub-investigator can sign the CRFs for assurance of the correctness and completeness of each page. DATA COLLECTION, CONTIN. (2) Any change or correction to a CRF should be dated, initialled and explained (if necessary) and previous/ original entries should not be obscured. This will allow for the maintenance of an audit trail. Draw a single line through the incorrect entry, not erasing, blacking out or using correction fluid; Write the correct information next to the original entry; Initial and date. Subject confidentiality should be protected to the possible extent. Although all trial documents should be appropriately identified by subject number and/ or date of birth (if applicable), reports sent to Company should make use of anonymised data. e.g. in some EU countries, MRI, CT scans and other source documents should not include direct and identificative patient data such as name, full DOB (year allowed) and patient initials. DATA COLLECTION, CONTIN. (3) The investigator must arrange for the retention and record of: -Patient identification codes (hospital / unit code, trial identification code and trial number) -Other source documents - patient files, clinic case notes and appropriate hospital records -Radiology or study specific data Radiology and Audiometric Data should be delivered to the Investigative Site for retention in the Subject Notes and / or Investigator Site File. If the Principal Investigator relocates or retires, Company must be notified (in writing). Trial documents and data including Site files should be retained for >15 years and, before destruction, Company must be informed by the Investigator. GCP AND REGULATORY COMPLIANCE DEFICIENCIES The most common deficiencies noted during Regulatory Authority inspections pertain to: •Inadequate medical records: should include information on disease/indication, legibility, concomitant diseases, patient included in study ID XXXX, written consent obtained, concomitant medication •Protocol non-adherence: inform CRA about all deviations, of problems to follow the protocol •Inadequate drug accountability: reconstitution, doses administrated, vials used per patient and dose and also concomitant medication •Improper consenting procedures: by Investigator, including copy of signed consent given to patient be signed and personally dated by the subject and by the person who conducted the informed consent discussion •Inadequate reporting of adverse events: Related or not related, significant or non-significant should be reported FDA WARNING LETTERS 2012 Number 1 Failure to ensure that the investigation was conducted according to the investigational plan, the signed agreement, applicable FDA regulations, and conditions of approval imposed by the IRB or FDA: (a) Failure to perform study visits at location specified in protocol (b) Failure to ensure that assessments were conducted by an individual qualified by credentials to do so (c) Failure to enroll subjects who met eligibility criteria (d) Failure to perform protocol required testing (e) Failure to perform protocol required testing within stipulated timeframes (f) Failure to comply with state regulations regarding the reporting of newly-identified HIV positive laboratory results to the Centers for Disease Control and Prevention (CDC) TACK! www.kvalitetsregister.se