Extravasation
Extravasation Is….
• Infiltration, tissuing, displacement………………..
- at the end of the day they are all the same injury
• The inadvertent administration of a cytotoxic drug,
targeted therapy or iodinated contrast agent into the
surrounding tissues, rather than into the vascular
pathway as intended.
• Vesicant extravasation is an oncological / parenteral
therapy emergency.
If we don’t take them seriously
Late PresentationVinorelbine
Extravasation..
Anthracycline Extravasation
(? Incomplete washout ? )
9 weeks after the event
Day 1
Day 7
Day 30
Often Difficult to Diagnose
• Extravasation?
• Flare reaction?
Flare reaction
• Flare reaction – red streak, flushing along the vein
•
•
•
•
•
Caused by an inflammatory response
Does not cause pain, although does cause ‘itching’
Usually the area is red and ‘blotchy’ (like nettle rash)
Occurs in 3 – 6% of patients
Often associated with
Doxorubicin
• Responds to topical steroids
• Usually resolves in over 85% of patients
within 45 minutes
Recognising an extravasation
1. Visual assessment
Initial
Redness/erythema
Swelling/oedema
Later
Inflammation
Induration
Exfoliation
Blistering
2. Patient reporting
Pain, discomfort
Burning, stinging
3. The infusion – warning signs!
The device alarms!
Increased resistance when administering drugs – BACK FLOW
Infusion becomes slow or sluggish
Schulmeister 2011, Doherty 2010
The Nature of Extravasation
Injuries Has Changed
• The most important development in the prevention and
management of extravasation is ‘the Chemotherapy Trained
nurse’.
• This has led to earlier detection of smaller volume
extravasations, and a greater appreciation of the hazard and
nature of the risk.
• This has diminished the potential consequences of the injury
and altered the intervention / observation dynamic.
• The average volume of drug extravasated in 1985 was 11.6mls,
in 1995 - 7.2mls and in 2005 - 3.1mls (www.extravasation.org.uk)
Extravasation Rate
• Statistics show that extravasations
occur in 0.5% - 6.5% of cytotoxic
administrations
(Albanell and Baselga 2000)
• Between 0.5% - 6% of cytotoxic drug
administrations will result in an
extravasation. (Dougherty and Oakley 2011)
How quickly should a vesicant
extravasation be washed out?
•Ideally within 6 hours
(Giunta 2004)
Surgical Intervention – The
‘Saline Wash Out Technique’
Gault 1993
Documentation!!!
• Need a complete history of the
extravasation event with diagrams and
photographs in the patient’s notes,
including the planned follow-up for the
patient.
• Follow up – what was the outcome?!
• PHOTOGRAPHIC EVIDENCE
Alternative to SWOT?
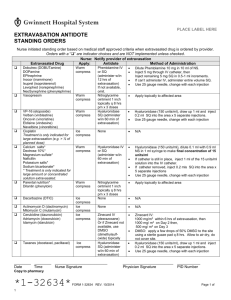
Antidotes……
Anthracyclines
Topical DMSO, corticosteroids
Mechlorethamine and Bendamustine
Sodium Thiosulphate (injected locally)
Vinca-Alkaloids
Hyaluronidase (inj localy)
Taxanes
Hyaluronidase
Schulmeister 2011, Doherty 2010, EONS 2007
Dexrasoxane (Savene)
• Only antidote licensed for anthracycline
extravasation
• Given as a peripheral infusion within 6 hours
of extravasation, then again at day 2 and 3.
• The anthracycline (full dose) then has to be re
given at day 4.
• Cost– around £6,000 per treatment ‘package’.
How can we help to minimize
the risk of extravasation?
• Do not site cannula in ACF or over bony
prominences
• Avoid multiple venepuncture!
• Avoid small fragile veins!
• Always cannulate distal to previous cannulation
• Take time when cannulating (view the whole arm!)
• Use a cannula placed specifically for purpose
• Vesicant first (if possible)
• Use a heat pad during administration
• Refer for a CVC before problems arise!!
Litigation?
• £22.5k compensation - woman left
scarred after chemotherapy drugs
leaked from a port catheter site during
treatment for breast cancer
Remember
• Extravasation is just one hazard of IV
chemotherapy – not directly life
threatening, but certainly has one of the
most serious long term consequences.
References..
National Extravasation Service
www.extravasation.org.uk (2007)
Dougherty
Extravasation: Prevention, recognition and Management
Nursing Standard (2010)
Vol 24, no 52, p 48-55
European Oncology Nursing Society (EONS)
Extravasation Guidelines Implementation Toolkit (2007)
http://www.cancernurse.eu/documents/EONSClinicalGuidelinesSection6-en.pdf
Gault D T
Extravasation Injuries
British Journal of Plastic Surgery (1993)
Vol: 46, no 2, p 91 – 96
Schulmeister L
Extravasation Management: Clinical Update
Seminars in Oncology Nursing (2011)
Vol 27, no1, p 82 – 90
Giunta R
Early sub cutaneous washout in acute extravasations
Ann Onc (2004)
15, p1146