969_File_6 - Bermuda Hospitals Board
advertisement

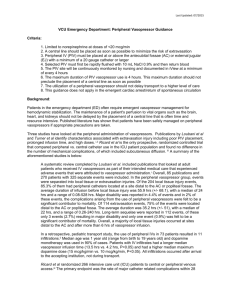
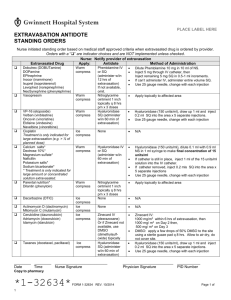
Vesicant Infusions A presentation for King Edward VII Memorial Hospital, Bermuda 23 January, 2012 Kristen Bodnaruk, RN, BS Denise Dreher, RN, CRNI, VA-BC Mary McCormick-Gendzel, RN, MS, CRNI, RN-BC Today’s Discussion: • • • • • • • Definitions Patient safety Peripheral and central VAD assessments Equipment Healthcare worker safety Drug administration Extravasation Definitions • Irritant: medication that may cause itching, phlebitis, or reaction along the vessel or at the injection site. • Vesicant: any IV drug that can cause blistering, severe tissue injury or tissue necrosis when extravasated. These may be chemotherapeutic or non-chemotherapeutic medications. Peripheral IV (PIV) Access • Gauge of catheter: ---bigger is not always better ---use smallest gauge possible to meet infusion needs ---smaller gauge decreases intimal damage and promotes hemodilution • Placement of catheter: avoid areas of flexion such as the hand, wrist, or antecubital fossa • Consider new PIV insertion daily if patient receiving daily vesicants • Start PIV insertions distally on arm and move proximally as therapy regimen progresses Risk Factors • • • • • • • Patient age, condition, or acuity Large gauge, location, and/or length of catheter Infusion history Poor VAD insertion technique Poor care and maintenance practices Extended dwell time Chemical makeup of drug: pH <5 or >9, osmolarity >600mOsm, or final dextrose concentration > 10% • Recent proximal peripheral venipunctures, or other existing PIVs in the same extremity Risk Factors • Recent proximal peripheral venipunctures, or other existing PIVs in the same extremity • Inadequate device securement • Confused or active patients could dislodge or damage access • Improper length of non-coring needle used with port access. • Inadequate device securement VAD Assessment • Patient comments/complaints • What is insertion date? (for PIVs) • Any swelling/edema noted…is transparent dressing looking taut?...is ID bracelet tight? • Is skin blanched or cool to touch? • Positive blood return? • Any redness (erythema) or leaking at insertion site? • Any difficulty flushing? • Radiological confirmation of central line catheter tip placement Some Potential Complications of Central Venous Access Devices (CVADs) • • • • • • Catheter occlusion Vessel occlusion Catheter rupture/fracture Device rotation Catheter migration For implanted ports: improper insertion of non-coring needle or needle dislodgement Equipment • IV tubing containing DEHP: (di-2ethylhexylphthalate) is a plasticizer added to PVC-based plastics to make them soft and pliable. There is evidence that certain drugs cause more leaching of DEHP. Increased amounts of DEHP in humans is concerning for its carcinogenic or hepatotoxic effects. Personal Protective Equipment (PPE) • Long-sleeved protective gown or cover-up should be lint-free and made of a low-permeability fabric. Gown should have a solid front, back closure, and tight cuffs. • Powder-free long-cuffed gloves designed specifically for chemotherapy should be worn. Gloves should be changed after each use, after 30 minutes of wear, or if they become torn or exposed to chemotherapy. • Face shield, goggles, or safety glasses should be worn Healthcare Worker Safety • • • • Proper handling of infusates and administration sets Caution with connecting and disconnecting Proper use of PPE Exercise caution when handling patient’s emesis, urine, or feces • Disposal of equipment into the appropriate biohazard bag or container • Follow established protocols and use a chemotherapy spill kit when cleaning up spills Vesicant Administration General Points of Emphasis • Continuous vesicants are given via central access. • Pre-filled administration sets versus backpriming of tubings • Vesicants are administered FIRST in a multiple chemo regimen • Patient education!! Pre-infusion • Informed consent? • Patient education: including signs/symptoms to notify RN if they feel any pain, burning, cool sensation, tingling, etc… at insertion site. • Gather supplies: ---clean pad or ‘chux’ to place supplies on at bedside ---PPE ---medication ---alcohol wipes ---empty 10ml syringe ---bag of 0.9% saline (NS) with tubing Pre-infusion • Check/double-check of correct medication and dosage per facility policies and procedures • Review of patient’s height, weight, body surface area (BSA), and any pertinent lab values • Patient identification using two verifiers Infusion • Do you have “the three C’s?”…. correct patient, correct medication and dose, and correct VAD? • Connect NS to VAD. Fluid should be fast and free-flowing. Chemotherapy should be connected at the lowest port closest to IV insertion site. Technique is known as “freeflowing side arm”. Infusion • When giving an IVP medication, blood return must be assessed every 2-3ml of infusate given. It should be given in a slow, steady push. • The NS should be free-flowing the entire time. • Site assessment should be on-going during administration. • End with NS flush of 100-200ml. Peripheral IV Extravasation Port Extravasation Port Extravasation Extravasation • Inadvertent administration of vesicant medication or solution into the surrounding tissue (INS, 2011) Extravasation • Any grade 4 infiltrate of a vesicant is considered an extravasation • Incidence is similar for peripheral and central line administration • Risk factors, such as fragile vessels, location of peripheral IV, or catheter integrity are things to consider • Antidotes may be used, but are considered controversial in some circles • Many non-chemotherapy agents have vesicant properties (e.g., Dopamine, Epinephrine, Gentamycin, Mannitol) Reference: MGH NPROM 08-02-01 Early warning signs of possible extravasation • • • • • • • Swelling Stinging, burning, or pain at insertion site IV flow that stops or slows Resistance when pushing medication Leaking around the port needle Lack of blood return Erythema, inflammation, or blanching Other symptoms/damage resulting from extravasation • Induration • Vesicle formation • Necrotic tissue damage can progress for six months • Tissue sloughing • Tendon, nerve, joint damage • Blistering at insertion site • Ulceration is usually seen 2-3 days to weeks following extravasation Treatment of Extravasation • IMMEDIATELY STOP INFUSION • Remove tubing from VAD, attach syringe to VAD, and aspirate drug • If via PIV, elevate extremity • Notify physician ASAP • Locate your institution’s policies or call Pharmacy for specific antidote • Application of heat or cold • Documentation in patient’s medical record • Documentation via safety report DNA-binding agents • Bind to the DNA in healthy cells when they extravasate into the tissue and cause cell death. • Retained in the tissue for long periods of time and cause progressive tissue necrosis. • Examples: anthracyclines (daunorubicin,doxorubicin, epirubicin, and idarubicin) • Application of cold 15-20 minutes for four to six times daily for 24 to 48 hours Non-DNA binding agents • Do not bind to the DNA in healthy cells, and are metabolized in the tissue • Examples: plant alkaloids (vincristine, vinblastine, and vindesine) • Application of heat 15 to 20 minutes for four to six times daily for 24 to 48 hours Some Available Antidotes • Totect (dexrazoxane) for anthracycline extravasation • Sodium thiosulfate for nitrogen mustard extravasation • Hyaluronidase for vinca alkaloid extravasation Helpful Websites • www.ins1.org • www.ons.org • www.cdc.gov/niosh References • Alexander, M., et al., Infusion Nursing. An Evidence-Based Approach. INS, Saunders, 2010. • Policies and Procedures for Infusion Nursing. INS, fourth edition, 2011. • Infusion Nursing Standards of Practice. INS, Lippincott, 2011. • Terry, et al. Intravenous Therapy: Clinical Principles and Practice. INS. WB Saunders, 2001 • Oncology Nurses Society (ONS) website • MGH Nursing Procedure Manual (NPROM) • MGH Clinical Policies and Procedures • MGH Infection Control Manual