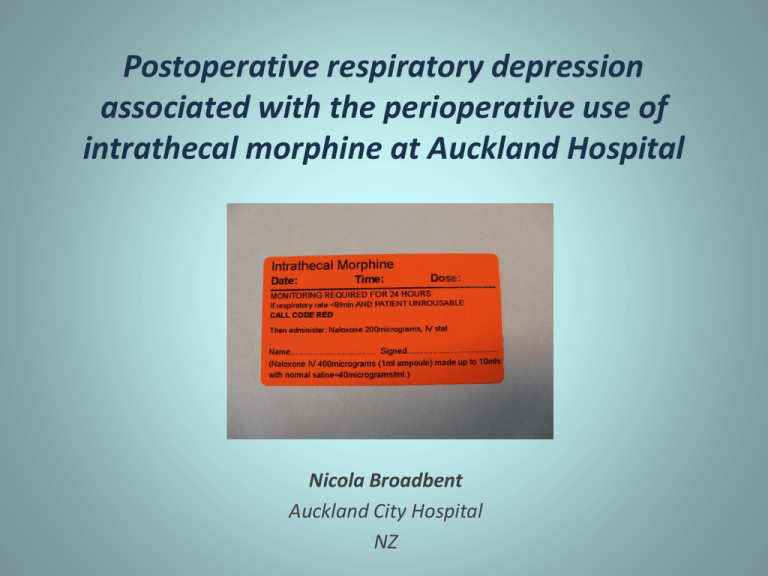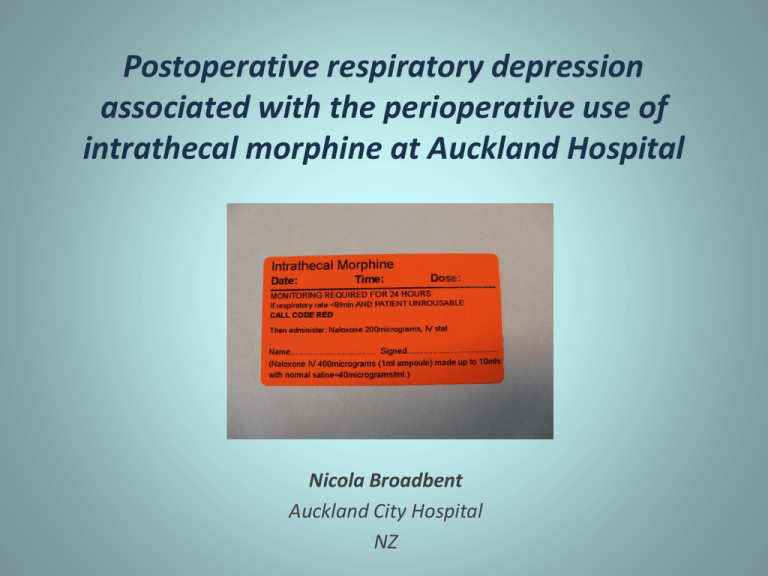
Postoperative respiratory depression
associated with the perioperative use of
intrathecal morphine at Auckland Hospital
Nicola Broadbent
Auckland City Hospital
NZ
Aims
To examine the usage of intrathecal morphine
at Auckland Hospital
Identify associated post-operative respiratory
depression and/or sedation
Design
Northern X Regional Ethics Committee
and ADHB Research Office approval
Retrospective 12 month period
– Sept 2008 - Sept 2009
Patient group
– Patients aged 16 years and over
– Single dose of intrathecal morphine
– Surgical procedures excluding obstetric
and cardiac bypass procedures
Controlled drug register
Notes review to confirm administration
Database compilation
Event data
• 24 hr period post intrathecal morphine dose
• Observations
–
–
–
–
Respiratory rate <8/min
SpO2<90%
GCS<9
Worst AVPU score
• Interventions
– Medical review
• sedation +/- respiratory rate
– Naloxone administration
– Code Red/Blue
– HDU/ICU admission
Patient characteristics
Total patients
429
Sex [n(%)]
Male
221 (51.5)
Female
208 (48.5)
Age in years [range(median)]
16-96 (70)
ASA score [n(%]
1
36(8.4)
2
218(50.8)
3
137(31.9)
4
19 (4.4)
5
0 (0)
Not recorded
19(4.4)
BMI (kg/m2) [range(median)]
*information available for 302 patients only
17.8-57.2 (27.6)
Obstructive sleep apnoea [n(%)]
7 (1.6)
Obstructive pulmonary disease [n(%)]
32 (7.5)
Other documented respiratory diagnosis [n(%)]
60 (14)
Surgical speciality
4 1
14 13
429 patients underwent 438 procedures
9 patients had 2 procedures
59
Orthopaedic (60.3%)
Urology(18.9%)
General surgery (13.5%)
Vascular surgery (3.2%)
Thoracic surgery (3%)
83
264
Gynaecology(0.9%)
No procedure (0.2%)
Anaesthesia
Patients [n(%)]
General anaesthesia
261 (59.7)
Regional anaesthesia+/- sedation
176 (40.3)
Elective procedure
361 (82.4)
Acute procedure
77 (17.6)
Intrathecal morphine dose
160
140
120
Dose range
Mean dose
Median dose
100
80
50-500mcg
158.5mcg
150 mcg
37 (8.4%) received a dose > 200mcg
60
40
20
Intrathecal morphine dose (mcg)
500
475
450
425
400
375
350
325
300
275
250
225
200
175
150
125
100
<100
0
Complications
Events
Procedures [n (%)]
Total events
53 (12.1)
Bradypnoea (RR <8/min)
47 (10.7)
Sedation with bradypnoea
16 (3.7)
Sedation without bradypnoea
5 (1.1)
SpO2 <90%*
2 (0.5)
Medical review for bradypnoea and/or sedation
15 (3.4)
Required intravenous naloxone
6 (1.37)
* 1 patient had preoperative hypoxia
Patients receiving naloxone
Intrathecal
morphine
dose (mcg)
Morphine
prior to ward
(mg)
RR < 8/min Sedation
Arterial blood gas
Time to
naloxone (hr)
54yr ♀
ASA not recorded
Partial hepatectomy
275
16
Yes
Yes
pH 7.33 PaO2 17.5 3.3
PaCO2 6.4 HCO3 23
61yr ♀
ASA 3
Hepatico-jejunostomy
250
4
Yes
Yes
pH 7.22 PaO2 12.1 11.5
PaCO2 7.9 HCO3 20
67yr ♂
ASA 2
Excision of hydatid liver cyst
275
10
Yes
Yes
pH 7.3 PaO2 11.1 14.5
PaCO2 7.0 HCO3 23
D 70yr ♂
ASA 2
Hepatico-jejunostomy
200
10
Yes
Yes
pH 7.23 PaO2 23.3 9.5
PaCO2 9.0 HCO3 24
76yr ♂
ASA 2
Partial hepatectomy
300
5
No
Yes
pH 7.25 PaO2 15.3 5
PaCO2 8.1 HCO3 23
80yr ♀
ASA 3
Nephro-uretectomy
150
3
Yes
Yes
pH 7.25 PaO2 21.1 10.5
PaCO2 7.4 HCO3 21
Opioid consumption
Route of administration
Procedures [n (%)]
Dose range (mg)
Intraoperative
46 (10.5)
1-20
PACU
62 (11.9)
1-30
Ward
9 (2.1)
1-7
Intravenous bolus morphine
PCA total
248 (56.6)
PCA morphine
197 (45)
PCA tramadol
30 (6.8)
PCA fentanyl
20 (4.6)
PCA pethidine
1 (0.2)
Oral opiates total
69 (15.8)
Sevredol
56 (12.8)
5-80
M-eslon
6 (1.4)
10-40
Oxynorm
6 (1.4)
10-30
Methadone
4 (0.9)
2.5-65
LA morph
1 (0.2)
200
Morphine infusion
4 (0.5)
Pethidine PCEA
1 (0.2)
Sedative co-analgesics
Analgesic
Procedures (n)
Naloxone adminstered [n (%)]
Gabapentin premedication
36
4 (11.1)
Intraoperative ketamine
25
0 (0)
Postoperative ketamine
9
0 (0)
Clonidine
4
0 (0)
Dexmedetomidine infusion
1
0 (0)
Events by speciality
Speciality
Procedures (n)
RR <8/min [n (%)]
Medical review
required [n (%)]
Naloxone given
[n (%)]
Orthopaedic surgery
264 (60.3)
14 (5.3)
2 (0.8)
0 (0)
Urology
83 (18.9)
10(12)
3 (3.6)
1 (1.2)
General surgery
59 (13.5)
19(32.2)
10 (16.9)
5 (8.5)
Vascular surgery
14 (3.2)
0 (0)
0 (0)
0 (0)
Thoracic surgery
13 (3)
4 (30.7)
1 (7.7)
0 (0)
Gynaecology
4 (0.9)
0 (0)
0 (0)
0 (0)
Aborted procedure
1 (0.2)
0 (0)
0 (0)
0 (0)
High incidence of events requiring intervention in general surgical group
– Hepatobilary patients responsible for all medical reviews and naloxone in this
group
Hepatobiliary subgroup
• Predominant group contributing to respiratory and sedation
events
– 36/37 received dose of 200mcg or greater
– Range 175-300mcg
– Mean 252 mcg
– Median 250mcg
Patients[n(%)]
Total
37
Gabapentin premedication
32 (86.4)
Morphine prior PACU discharge
19 (51.4)
RR < 8/min
13 (35.5)
Medical review
10 (27)
Naloxone
5 (13.5)
Unplanned HDU admission
4 (10.8)
How does this audit fit in the
literature?
Author
Year
published
Type
Country
No of
patients
Respiratory
depression
NNH
Tramer et al
2009
Meta-analysis
Multiple
645
1.2%
84
Lim et al
2006
Audit
Australia
407
0.2%
Gwirtz et al
1999
Audit
USA
5969
3%
Rawal et al
1987
Survey
Sweden
~1103
0.38%
Gustafsson et al
1982
Survey
Sweden
~90-150
4-7%
275
In summary
• In this retrospective QA project
– 12.1% had a respiratory or sedative complication
– 3.4% triggered a medical review
– 1.37% needed iv naloxone for respiratory depression +/- sedation
• Features
– Respiratory depression delayed 3.3-14.5 hr post dose
– General surgical/hepatobiliary patients over-represented
•
•
•
Larger intrathecal morphine doses
Early iv morphine prior to PACU discharge
Gabapentin premedication
• Conclusions
–
–
–
–
Orthopaedic patients can be nursed in ward setting with appropriate observations
Consider HDU placement for general surgical/hepatobiliary patients
Caution with early opiates and consider short acting opiates (eg fentanyl) for bridging
Caution with gabapentin premedication
Optimum dosing
• Optimization of the Dose of Intrathecal Morphine in Total Hip
Surgery: A Dose-Finding Study
• Robert Slappendel et al. Anesth Anal 1999 88:822-6
– 143 pt receiving either 25,50,100,200mcg followed for 24hr
– Optimal dose as low as 0.1mg.
– 0.2mg did not improve analgesia but increased side effects
• Optimizing the dose of Intrathecal Morphine in Older Patients
Undergoing Hip Arthroplasty
•
Laffey et al Anesth Anal 2003. 97: 1709-15
–
–
•
60 pt receiving either 0, 50, 100, 200mcg followed for 24hr
100mcg morphine provides best balance between analgesic efficacy
Minimal effective dose of Intrathecal morphine for Pain Relief
Following Transabdominal Hysterectomy
•
Watanabe et al Anesth Anal 1989
–
–
188 pt receiving 30,40,60,80,100mcg followed for 48hr
Effective analgesia at 40mcg.
Hepatobiliary patients in the literature
• 2 recent studies
• The use of intrathecal morphine for postoperative pain
relief after liver resection: A comparison with epidural
analgesia
– De Pietri et al Anesth Anal 2006
• A change in practice from epidural to intrathecal
morphine analgesia for hepato-pancreato-biliary
surgery
– Sakowska et al World J Surg 2009
Defining respiratory depression
• What do we mean?
– Inadequate ventilation?
– Bradypnoea?
– Failure to oxygenate and clear waste gases?
• What can we measure on the ward?
• Definitions of "respiratory depression" with intrathecal morphine
postoperative analgesia: a review of the literature
– Goldstein et al. Can J Anesth 2003
– 96 studies
– 46% did not define “respiratory depression” when used
– 25% defined by respiratory rate alone
• SpO2, ABG, naloxone treatment, carbon dioxide stimulation, level of sedation
Data collected
•
Patient demographics
•
Intrathecal morphine dose
•
Surgical and anaesthetic details
•
Other opioids
– Early morphine consumption
• prior to PACU discharge
– Presence/absence of PCA
– Opioid usage over 24hr
•
Sedative co-analgesics
– Gabapentin premedication
– Ketamine
– Clonidine
– Dexmedetomidine
•
Pain scores
Bradypnoea (APS guidelines)
• Local guidelines recommend treatment with
naloxone if RR <8/min and unrousable
• 5.2% had a RR of <8/min documented
– 1.7% on surgical ward
– 1 given naloxone