Intern Boot Camp Abdominal Pain
advertisement
Joshua Sapkin, MD
Associate Program Director
LAC+USC Internal Medicine Residency Program
Lecture Goals
Review the various etiologies of dyspnea by organ
system
Review the most common cardiac and pulmonary
etiologies of hypoxia
Utilize the A:a gradient to determine the correct
pathophysiology responsible for a patient’s hypoxia
Appreciate the systematic approach that should be
taken to evaluate a dyspneic patient
Appreciate the roles, including limitations, of various
diagnostic tests
Etiologies
Cardiac
Pulmonary
Mixed cardiac and pulmonary
Psychiatric (e.g. anxiety, panic disorder)
Cardiac Etiologies
Congestive heart failure
Systolic dysfunction
Diastolic dysfunction
Valvular heart disease
Hypertrophic obstructive cardiomyopathy
Cardiac tamponade
Tension pneumothorax
Intracardiac right to left shunting
Arrhythmias
Bradydarrhythmias
Tachyarrhythmias
Pulmonary Etiologies
V/Q mismatch
Shunt
Diffusion barrier
Hypoventilation
Altitude
V/Q Mismatch
The most common pathophysiology leading to
hypoxemia.
Atelectasis
Chronic bronchitis
Pneumonitis
Pneumothorax
Pleural effusion
Pulmonary edema
Shunt
Pulmonary embolus
Acute lung injury
ARDS
Hepatopulmonary syndrome
Right to left intracardiac shunts
Hypoventilation
Opiate analgesics
Benzodiazepines
Barbiturates
Asthma
Emphysema
Central disorders
Diffusion Barriers
Interstitial lung disease
Medication induced, e.g. nitrofurantoin, sulfasalazine,
amiodarone,
Illicit drugs, e.g. heroin
Cryptogenic organizing pneumonia
Lymphocytic interstitial pneumonia
Non-specific interstitial pneumonitis
Lymphangioleiomyomatosis
Connective tissue disease
Sarcoidosis
Infectious
Hypersensitivity pneumonitis
Other Etiologies
Severe kyphoscoliosis
Neuromuscular disorders, e.g. myasthenia gravis
Altitude
Carbon monoxide poisoning
Severe anemia (usually fairly acute)
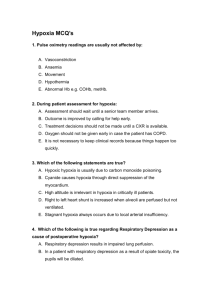
Question 1
Which of the pathophysiologies responsible for
dyspnea is not associated with an increased A:a
gradient:
A.V/Q mismatch
B. Shunt
C. Diffusion barrier
D. Hypoventilation
Alveolar:arterial gradient
A-a gradient = predicted pO2 – observed PO2
PAO2 = (FIO2 X 713) – (PaCO2/0.8) at sea level
PAO2 = 150-(PaCO2/0.8) at sea level on room air
“Poor man’s” A:a gradient (ABG must be performed
on room air): 140-pCO2-pO2
Normal= {Age÷ 4} ₊ 4
Case 1
The nurse calls you because your patient who had a left
subclavian central venous catheter placed 1 hour ago is
complaining of shortness of breath. The patient is a 55
year old man who was admitted for left leg cellulitis
that was refractory to oral antibiotics.
Case 1
Which of the following diagnoses is most likely?
A. Pneumocystis Jaroveci pneumonia
B. Pulmonary embolus
C. Intrapulmonary hemorrhage
D. Pneumothorax
Case 1
Upon arriving at the patient’s bedside, you find him in mild
respiratory distress.
Vital signs: Blood Pressure: 144/82. Heart rate 100.
Respirations: 24. Temperature: 98.2. Oxygen saturation
94% on room air.
P.E. HEENT: Anicteric. No conjunctival pallor.
Neck: No JVD.
Cardiac: Tachycardic.
Chest: Trachea midline. Lungs clear to auscultation
Abdomen: Non-tender, non-distended. No
organomegaly.
Be careful of the pulse oximeter
Case 1
What is the next best step in the management of this
patient?
A. Chest X-ray
B. V/Q scan
C. HRCT of the lungs
D. Echocardiogram
Case 1
Case 1
Why are vital signs called “vital” signs?
A. They are a necessary component of the medical
documentation in order to bill health insurances
(vital for reimbursement)
B. They are important clues to the patient’s diagnosis
(vital for establishing a diagnosis).
C. The nurses consider them essential pieces of
information before paging a physician (vital for
paging a physician)
D. They reflect physiologic processes that are essential
to sustaining life.
Case 1
All of the following measures would be appropriate a this
time EXCEPT:
A. Check the patient’s blood pressure in the supine and
sitting position.
B. Ensure the patient has two large bore peripheral IV
sites.
C. Contact the GI fellow who performed the procedure.
D. STAT General Surgery consult
E. Ask the nurse if he/she would like to join you for a drink
at Barbara’s Brewery after work.
Case 1
Case 2
The nurse pages you because your patient has a respiratory rate of 6 and an oxygen
saturation of 85% on room air. He is a 42 year-old man with history of IVDU who was
admitted for multiple abscesses and cellulitis affecting both upper extremities. He had
been off the ward for 3 hours. His nurse noticed that he seemed under the influence of a
substance upon returning to his room about 1 hour ago.
P.E.
Height: 5’ 9” Weight: 140 lbs.
Vital Signs: Blood pressure: 100/62. Heart Rate: 110 Respirations: 6. Temperature: 99.0.
Pulse oximeter 85% on room air.
General: The patient does not respond to verbal or painful stimuli.
HEENT: Pinpoint pupils. Sluggish response to light. There is dried food at the borders of
the mouth.
Neck: No JVD.
Tachycardic . No murmurs, rubs or gallops.
Chest: No deformities. There are decreased breath sounds over the right lower lung field.
Case 2
The next best step in the management of this patient
is:
A. Naloxone intravenously
B. Sternal rub
C. Call the airway team
D. Ventilate the patient using a bag valve mask (BVM).
Case 2
The ABG prior to hyperventilating the patient revealed
the following:
7.58/60/58/24/85%
What is the calculated A:a gradient?
What is the expected calculated A:a gradient?
Case 2
What is the calculated A:a gradient?
140-pCO2-pO2 = 140-60-58=22
What is the expected calculated A:a gradient?
Age 42: [42÷4] ₊ 4= 14
Case 2
Case 3
A 67 year-old woman is found to have an oxygen
saturation of 88% by her nurse 4 days after undergoing
bilateral total knee arthroplasties. Vital Signs: BP
120/72. Pulse 100. Respirations 20. Temperature 99.4.
Exam is significant for inspiratory rales over bilateral
bases. ABG: 7.46/35/64/20/88%
Case 3
Which piece of data provides the best evidence that
this woman does not have a partial small bowel
obstruction?
A. Her cholecystectomy was performed 20 years ago.
B. The timing and duration of her symptoms
C. The results of her abdominal series
D. Her abdominal exam
Case 3
Case 3
Which of the following statements is true regarding
pulmonary emboli?
A. V/Q scan is the gold standard for establishing this
condition.
B. A confirmatory CT angiogram should be performed
before starting anticoagulation.
C. The D-dimer test is a highly sensitive and specific
test for this condition.
D. The ECG usually demonstrates evidence of right
heart strain during an acute pulmonary embolus.
Case 4
A 75 year old woman with essential hypertension left
ventricular hypertrophy (hypertensive heart disease),
diabetes and long history of smoking undergoes
surgical repair of a 7 cm aneurysm of the descending
aorta. She develops hypoxia on post-operative day #1
requiring 4 liters of oxygen via nasal cannula to
maintain her oxygen saturations above 90%. Exam is
significant for elevated jugulovenous pressure,
scattered expiratory wheezes, decreased breath sounds
over the bases and 1+ pitting edema over bilateral
lower extremities.
Case 4
Which piece of history is most pertinent to
establishing the cause of her hypoxia?
A. Her net fluid intake/output over the past 24 hours.
B. The number of pack-years she has smoked in her
lifetime.
C. The length of the surgery.
D. The total amount of opiate analgesics administered
since surgery.
Case 4
All of the following diagnostics can help distinguish
between a pulmonary and cardiac cause of dyspnea
EXCEPT:
A. B type natriuretic peptide
B. Chest x-ray
C. Oxygen Extraction Ratio VO2/DO2 x 100
D. Pulmonary capillary wedge pressure