Congenital Heart Defects - Macomb
advertisement

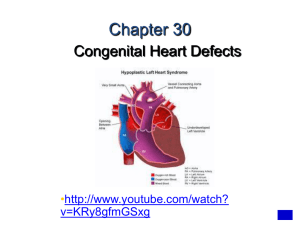
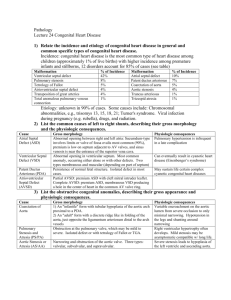
Congenital Heart Defects MODULE F Chapter Eleven Cardiac System Pages 348 - 359 Objectives • Differentiate between the different congenital heart diseases and state whether they are cyanotic and acyanotic. • Describe the defect present with each congenital heart disease. • Describe the surgical repair (if any) for each congenital heart disease. Cardiac Defects • • • • • • • • • Patent Ductus Arteriosus Atrial Septal Defect Ventricular Septal Defect Tetralogy of Fallot Transposition of the Great Arteries Coarctation of the Aorta Anomalous Venous Return Truncus Arteriosus Hypoplastic Left-Heart Syndrome Web Sites • http://www.childrensheartinstitute.org/edu cate/defects/defects.htm Normal Cardiac Blood Flow Ductus Arteriosus • Fetal Circulation Component • Connects Pulmonary Artery to Aorta • Shunts blood away from lungs • Maintained patent by presence of prostaglandins • Closure secondary to: • Increase in PaO2_ • Decrease in level of prostaglandins Patent Ductus Arteriosus • 5-10% of all births (1 of 2000 live births) • 80% of premature babies • 2-3 times more common in females than males. • 5th or 6th most common congenital cardiac defect. • Often associated with other defects. • May be desirable with some defects. • Morbidity/Mortality related to degree of blood flow through PDA. Pathophysiology - PDA • With a drop in pulmonary arterial pressure (reduction in hypoxic pulmonary vascular constriction), blood will flow through PDA. • LEFT TO RIGHT SHUNT • Increased pulmonary blood flow may lead to pulmonary edema. • Reduced blood flow to all postductal organs • NEC • If pulmonary artery pressure rises above Aortic pressure, blood will move in the other direction. • RIGHT TO LEFT SHUNT Diagnosis - PDA • Loud grade I to grade III systolic murmur at left sternal border. • Washing machine • Echocardiography Treatment - PDA • • • • Restrict fluids. Diuretics Prostaglandin Inhibitors - Indomethacin Surgical closure (ligation). Atrial Septal Defect • 6-10% of all births (1 of 1500 live births) • 2 times more common in females than males. • Types: • Ostium Secundum (at or about the Foramen Ovale) • Sinus Venous (at about the point where SVC and IVC attach to Right Atrium) • In 1950 most children with ASD did not reach the first grade. Today, first year surgery facilitates normal growth and development. ASD: Pathophysiology and Diagnosis • Pathophysiology • Left to Right Shunt • Inefficient recirculation of good blood through pulmonary arteries. • May not manifest symptoms and may be found later in life. • If defect is significant, may cause problems later in life due to inefficiencies. • Diagnosis • Murmur • Echocardiography Treatment - ASD • Surgical closure. • Non-Surgical closure via cardiac catheterization. Ventricular Septal Defect • 1% of all births (2 to 4 of 1000 live births) • Vast majority the hole is small. • In 1950, fatal. Today almost all VSD can be closed successfully, even in small babies. Lillehei was the first person in history to correct both ASD and VSD on 8/31/54. VSD: Pathophysiology & Diagnosis • Pathophysiology • May be isolated or associated with other congenital cardiac defects. • With normal PVR: • LEFT TO RIGHT SHUNT • With elevated PVR (RDS): • RIGHT TO LEFT SHUNT • Diagnosis • Echocardiography Treatment - VSD • Nothing if VSD is small. • With CHF or Failure to Thrive: Surgical closure. http://64.143.41.32/news.html Tetralogy of Fallot • 1% of neonates. • Most common of the cyanotic cardiac diseases. • Mortality increases with age (1 year-old has a 25% mortality, 40 year-old has 95%). • In 1950, fatal. Today, less than 5% mortality with children operated on in infancy, leading normal lives. Four Defects • Pulmonary Artery Stenosis (determinant factor related to severity) • VSD (usually large) • Overriding Aorta • RV hypertrophy Tetralogy of Fallot: Diagnosis and Treatment • • • • Tet Spells CXR: Boot-shaped Heart Diagnosed with echocardiography. Surgical correction. • Reparative or Palliative (Blalock-Taussig) Blalock-Taussig • Something the Lord Made. • Vivien Thomas Complete Transposition of the Great Arteries • Second most common form (5-7%) of congenital cardiac anomalies. • Aorta arises from RV and Pulmonary Arteries from LV. • Without an abnormality, life would not be possible. • ASD • VSD (30-40%) • PDA Transposition – Diagnosis and Treatment • Diagnosis • Chest X-Ray: “Egg on a String” • Echocardiography • Cardiac Catheterization (?) • Treatment • Balloon septostomy during cardiac cath. • Rashkind’s Procedure • Reestablish Foramen Ovale • Prostaglandin E1 to keep PDA open. • Surgical Correction • Jantene Operation Coarctation of the Aorta • 7% of congenital cardiac defects. • Constriction of the aorta. • Results in severely reduced blood flow. • Increased work on the heart leading to CHF and cardiovascular collapse. • Location of narrowing determines the clinical signs. • Usually associated with PDA, VSD and a defective aortic valve. Location of Coarctation • Pre-Ductal • Less common but more serious • Associated with VSD, PDA, Transposition • Post-Ductal • More common • Often associated with collateral circulation beyond coarctation, which minimizes effect. • Diagnosed by a difference in blood pressure between lower extremities and upper ones. • Pressure in upper extremities > lower Coarctation – Diagnosis and Treatment • Diagnosis • Chest X-Ray • Echocardiography • Cardiac catheterization • Treatment • Support with inotropic agents (Dopamine). • Prostaglandins to maintain PDA. • Surgical repair Anomalous Venous Return • Return of pulmonary venous blood to the right atrium instead of the left. • ASD is present to sustain life. • Can also be partial. • Cyanosis usually present. • Diagnosed with echocardiography. • Surgical correction with reimplantation of pulmonary veins. Truncus Arteriosus • Defect in which one large vessel arises from right and left heart over a large VSD. • Cyanosis is often present. • CHF common. • Diagnosed with echocardiography and cardiac catheterization. • Surgery: • Separate pulmonary arteries from truncus. • Closure of VSD • Create valved connection between RV and Pulmonary Artery Repair of Truncus Arteriosus Hypoplastic Left-Heart Syndrome • Several anomalies: • Coarctation of the aorta • Hypoplastic left ventricle • Aortic and mitral valve stenosis or atresia. • Cyanotic defect. • Right heart pumps blood to body through PDA. • Closure of PDA results in hypotension, shock, and death. • Maintain hypoxemia with normalized CO2 levels. • “40-40 Club” 1 Patent foramen ovale 2 Coarctation of the aorta 3 Patent ductus arteriosus 4 Narrowed aorta 5 Hypoplastic left ventricle 6 Aortic atresia Surgical Treatment of Hypoplastic Left Heart Syndrome • Three separate surgeries. • Norwood procedure • First few days after birth. • Glenn Shunt (Cavo Pulmonary Connection) • 3-9 months of age • Fontan Procedure • 2 years of age • Less wait because of damage from pulmonary hypertension. Stage I - Norwood Procedure Stage II - Glenn Shunt Stage III – Fontan Procedure