kamcampusCS2
advertisement

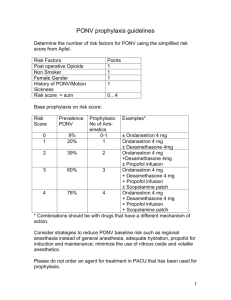
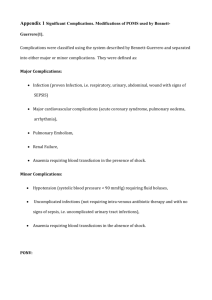
Running head: Postoperative Nausea and Vomiting Postoperative Nausea and Vomiting Kam Campus Wolford College 2013 A kamcampus@gmail.com Running Head: PONV Postoperative nausea and vomiting (PONV) is a prevailing complication in anesthesia. According to Barash, approximately 35% of patients who receive anesthesia experience PONV. The exact mechanism of PONV is not clearly understood, but several risk factors have been identified such as the use of narcotics, nitrous oxide and inhalation anesthetics. Patients who are high risk for PONV should receive a prophylactic antiemetic. The goal of prophylactic treatment is to prevent PONV however this method is not fail safe. A.S. was a 5’3”, 73 kilograms, and 51 years old Caucasian female. She presented to the E.R with complaints of nausea, vomiting, and abdominal pain for four days. An abdominal CT scan revealed cholecystitis. A.S. was admitted and scheduled for a laparoscopic cholecystectomy. The patient was prescribed anti-emetics and intravenous fluid replacement prior to surgery. She was generally healthy; coexisting diseases included depression and anxiety, which the patient stated were well controlled with medications. Lab values were not significant, chest X-ray was normal, and her 12 lead EKG revealed SR 72 bpm. On evaluation, A.S. denied any significant medical history. Past surgical history included two C-sections with no anesthetic complications. The patient’s airway assessment revealed natural dentition, Mallampati (MP) 2, thyromental distance (TMD) 3 finger breadths (FB), mouth opening > 4 cm, and full range of motion (FROM) of the neck. ASA II was selected for this patient. A.S. was treated in the preoperative holding area with Midazolam 2 mg IV. The patient was taken to operating room (OR) where ASA monitors were applied. She was preoxygenated with 10L of O2 via facemask prior to induction. A.S. was positioned Running Head: PONV supine with arms abducted < 90 degrees. All pressure points were padded appropriately. Fentanyl 50 mcg, 1% Lidocaine 50mg and Propofol 200mg IV were administered. Upon loss of verbal and eyelid response, the patient was successfully bag-mask ventilated, which was followed with Succinylcholine 100mg IV. Using the MAC 3 blade, a #7.0 ETT was successfully inserted as evidenced by chest rise, condensation in the tube, EtCO2, and bilateral auscultation of breath sounds. Sevoflurane was started at 3% with volume control ventilation. Following induction, the patient’s blood pressure decreased slightly. Sevoflurane was decreased to 2%. Because of the patient’s history of recent vomiting, dexamethasone 10mg IV and ondansetron 4 mg IV were given intraoperatively in effort to prevent PONV. Maintenance of the case was uneventful. Upon conclusion of the case, Sevoflurane was discontinued and the O2 was increased to 10L. The patient met the criteria necessary for extubation such as hemodynamic stability, adequate spontaneous ventilations, intact airway reflexes and ability to follow commands. She was suctioned prior to extubation and transferred to PACU on 2L via nasal cannula. The purpose of this case study is to examine PONV and it’s impact on patients receiving anesthesia. The rationale is to minimize or prevent PONV. According to a survey that concluded prevention of PONV is crucial for the operative patient. Additionally, they concluded that lack of PONV was correlated with higher patient satisfaction scores (Ting, 2005). Unfortunately, many anesthetics contribute to PONV such as inhalation agents, nitrous oxide and narcotics. Aggressive prevention of PONV may be expensive but desired in the ambulatory setting to maintain patient satisfaction scores. Running Head: PONV According to Ting, a risk stratification system to identify patients at high risk for PONV is important to implement. Certain patient attributes are associated with a higher risk of PONV such as female gender, younger age, non-smokers, obesity, and history of motion sickness. Furthermore, specific types of surgeries predispose patients to PONV such as gynecologic, laparoscopic, and intra-abdominal surgeries. The anesthesia provider should consider each patient and procedure when assessing his or her risk for PONV. Most anesthesia providers can use their clinical experience and knowledge of the particular case and anesthesia required to stratify the patient as high, medium, or low risk for PONV. Patients who are low risk for PONV should receive no prophylactic treatment or minimal treatment. Patients at medium risk for PONV should receive a prophylactic treatment and if PONV occurs it should be treated aggressively. The patients who are identified as a high risk for PONV should receive aggressive prophylactic treatment. Additionally for the high-risk group, Ting recommends using a concept of multi-modal therapy. This concept includes the use total intravenous anesthesia, avoidance of drugs known to be associated with PONV, aggressive anti-emetic prophylaxis using drugs with different mechanisms of action and aggressive fluid replacement. A comprehensive patient evaluation including patient’s comorbidities, type and duration of surgical procedure should be considered when determining the anesthetic plan. In this particular case, I would consider the patient to be at high risk for PONV due to her recent history, the scheduled laparoscopic procedure, and the use of inhalation agents. A.S. did receive prophylactic treatment including dexamethasone 10mg and ondansetron 4mg. After reviewing this topic, I would have given a third prophylactic drug such as metoclopramide. All three anti-emetics mentioned work on different Running Head: PONV receptors in chemotrigger receptor zone. It is important to be knowledgeable of the medications we use to provide the best care possible to our patients. References Barash, PG., Cullen, BF., Stoelting, RK., Cahalan, MK., & Stock, MC. (2009). Clinical anesthesia. (6th ed.). Philadelphia, PA: Lippincott,Williams, & Wilkins. Ting. (2005). Postoperative nausea and vomiting (PONV): an overview. Anesthesiology Info. Retrieved from http://anesthesiologyinfo.com/articles/04252004.php