What*s New with PONV & PDNV?
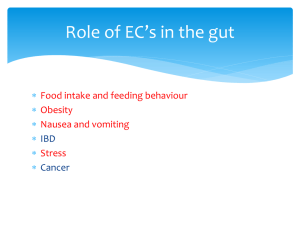
advertisement
What’s New with PONV & PDNV? 1100 - 1200 Objectives • Describe ASPAN EBP postoperative nausea and vomiting (PONV) and Post discharge nausea and Vomiting (PDNV) clinical practice guideline • Describe algorithm for prevention and treatment of nausea and vomiting. PONV/PDNV * Clinical Practice Guideline 3 in Part IV of ASPAN Standards • Most common complication affecting 1/3 of surgical patients (75 million individuals) • PONV is a strong predictor of: – Prolonged postoperative stay – Unanticipated admissions – Financial impact • Costs several million dollars each year ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 PONV • Reported as – Common fear prior to elective surgery – More debilitating than postop pain or surgery itself • Adverse impact of PONV & PDNV include – – – – – – Aspiration Wound dehiscence Prolonged hospital stay Unanticipated hospital admission Delayed return of patient’s functional ability Lost time from work for patient & caregiver ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Definitions NAUSEA Subjective report of an unpleasant feeling in the epigastrum &/or in the back of the throat “Feeling sick to my stomach” ”Feeling queasy” “Turning stomach” “Feeling squeamish” VOMITING Forceful expulsion of contents of stomach, duodenum & jejunum through the oral cavity as a result of change in intrathoracic pressure “Puking” “Upchucking” “Throwing up” “tossing my cookies” “Barfing” ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Postoperative Nausea & Vomiting • N&V that occurs within the first 24 hours following surgery – Early: 2-6 hours after surgery ( in PACU) – Late: 6-24 hour period – Delayed: Occurs beyond 24 hours in inpatient setting • POSTDISCHARGE NAUSEA & VOMITING (PDNV) – Nausea & vomiting that occurs after discharge – Occurs beyond the initial 24 hours after DC ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Risk Factors for PONV • Supported by Strong evidence – – – – – – – Female gender History of PONV History of motion sickness (Subjective) Non-smoker Postoperative use/administration of opioids Use of volatile anesthetics Use of Nitrous Oxide • Supported by weak evidence – Age – Duration of surgery • Supported by conflicting evidence – Type of surgery ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Interventions • Prophylaxic – Antiemetic strategies implemented PRIOR to onset of symptoms – Anesthesia considerations: TIVA, NSAIDs, Regional blocks • Pharmacological – Prescribed medications used to prevent &/or treat N&V – Dexamethasone – 5HT3 receptor antagonists – H1 receptor blockers (antihistamines – Scopolamine patch – Droperidol – New drug class: Neurokinin (NK1) antagonists Interventions • Therapeutic: – Treatment options other than meds, requiring physicians order, that are commonly used for management of PONV/PDNV – Hydration – Pain management • Complementary – Non-conventional treatment options used in conjunction with traditional or conventional therapy in management of N&V – Aromatherapy, Herbals, Acupressure ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Preadmission Testing/ Preop Holding • Assess for PONV/PDNV risk factors • Document and communicate risk factor assessment – identify prior to surgery • Prophylactic recommendation intervention based on: – Efficacy of interventions • Consideration of success rate • Duration of action – Risk of developing side effects, or number &/or severity of side effects – Cost ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 PONV Prophylaxis Recommendation • Prophylaxis for PONV: – Anesthesia considerations • Tiva, NSAIDs, Regional blocks – Pharmacological • Dexametasone, 5HT3 receptor antagonists, H1 receptor blockers, Scopolamine patch, Droperidol, Neurokinin – Therapeutic • Hydration (clear liquids 2 hours prior to surgery); Supplemental IVs • Pain management: NSAIDs, Regional – Complementary • P6 Acupoint stimulation Postoperative Phase I/ II Management • Assess for postop N&V (High risk if opioid use) • If nausea present quantify severity • Implement rescue interventions – Verify adequate hydration and blood pressure – Select & administer appropriate rescue anti-emetic • 5-HT3 receptor antagonists, H1 receptor blockers, Droperidol, Metoclopramide, low dose promethazine, prochloroperazine – New drug class: Neurokinin antagonist – Consider aromatherapy ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 Postdischarge N&V Recommentaions • Assess for PDNV risk factors • Administer prophylactic antiemetics in high risk – Dexamethasone, Scopolamine patch, • Complementary interventions • Patient education on management • Rescue treatment – Antiemetic strategies implemented AFTER the onset of symptoms • Rescue treatment for PDNV may include – Ondansetron dissolving tablets, Promethazine suppository or tablets, Scopolamine patch ASPAN Clinical Practice Guideline for Prevention &/or Management of PONV/PDNV 2010 NAUSEA & VOMITING • PHYSIOLOGY – Neuromuscular interaction – Emetic Center • Vagal viscera • Sympathetic viscera • Vestibular • Cerebral Cortex/Limbic • Chemoreceptor Trigger Zone (CTZ) Physiology of Vomiting: Neurotransmitters Sensory input Higher centers Cerebellum HM Solitary tract nucleus SDMH M=Muscarinic cholinergic receptors H = Histaminergic receptors D = Dopaminergic receptors S = Serotonergic receptors Vomiting center SDM Chemoreceptor trigger zone DS Upper gastrointestinal tract Inner ear vestibular apparatus Toxins in blood and CSF Brunton LL. In: Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 1996;917-936. NAUSEA & VOMITING • RISK FACTORS – Anesthetic Agents – Hypotension – Variables in patients – Surgical Procedure – History – PAIN ANTIEMETICS • Chlorpromazine (Thorazine) • • Dimenhydrinate • (Dramamine) • Meclizine (Antivert, Bonine) • • Metoclopramide (Reglan) • • Droperidol (Inapsine) • Hydroxyzine (Vistaril) • • Diphenhydramine (Benadryl) • • Alcohol –aroma therapy • Quease ease – aroma therapy • • Ephedrine Ondansetron HCL (Zofran) Dolasetron (Anzemet) Graniseton (Kytril) Prochloperazine (Compazine) Promethazine (Phenergan) Trimethobenzamide HCL (Tigan) Transdermal Scope Comparative Receptor Affinities of Antiemetic Drug Classes Receptor Affinity Antiemetic Drug Class Dopamine Anticholinergic agent + ACH Histamine Seroton ++++ + Antihistamines + ++ ++++ Phenothiazines ++++ ++ ++++ Butyrophenones ++++ + Benzamides +++ + Selective Serotonin Antagonists ++++ Ouellette SM. CRNA. 1999;10:24-33. Postoperative Patient Management • Expected Outcomes – Routine assessment – Appropriate PONV rescue treatment – Incidence of PONV will be reduced – Incidence of rescue will be reduced – Patient satisfaction will be improved – Time and cost of patient’s return to normal activities will be reduced – Outpatient education and follow-up QUESTIONS??