PowerPoint_Format
advertisement
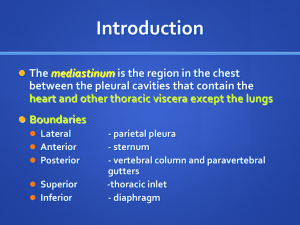
Dr Rafaat, can you do one CT guided Biopsy before you go home? What I knew: HPI: 15 year old, 60kg female, presenting to outside hospital with a 10 day history of fatigue, dyspnea and cough Additionally, had HA, night sweats and weight loss PMHx: ex 26wk preemie, some “EKG abnormality”, recent hx of recurrent PNA SurgHx: s/p PDA ligation Something was going to be biopsied. CT scan was from outside hospital, and was not in EPIC What I knew: It was 5pm, most of ASMG had gone home, and CT is FAR AWAY from the OR AND I sent the resident home, because this was “just a biopsy” What I Discovered: 11 x 7 x 11cm Anterior mediastinal mass Look at it, gently covering the trachea and SVC. Normal Structures in CT • Marked compression of SVC with obstruction • Mild compression of branch PAs without obstruction • Right Pleural effusion Compression, without occlusion of bilateral mainstem bronchi Compression, right bronchus Mediastinal Compartments Mediastinal Masses Of all mediastinal masses, 35%-55% arise in the anterior mediastinum The most common types of tumor in the anterior mediastinum are known by the Four “T”s: Teratoma Terrible Lymphoma Thyroid Thymoma From Lerman, J Anterior Mediastinal Masses in Children, Semin Anes, Peri Pain, (26) 2007 EKG Guesses? Wolff-Parkinson-White Syndrome Due to an accessory pathway that bypasses AV node allowing reentry tachyarrhythmias Pts at risk for PSVT and AF Anesthetic management involves avoiding increases in sympathetic tone Treat anxiety and pain Maintain adequate intravascular volume Avoid medications that may precipitate tachycardia (Ketamine, Glyco, Epi) Neostigmine, by slowing conduction through the AV node, may encourage conduction through accessory pathway Treatment is with Calcium channel blockers, beta blockers NOT ADENOSINE ( can induce VF) Echo Echocardiogram showing SVC occlusion by the mass. RV was under filled. Echo otherwise showed preserved LV function and findings consistent with CT. What I Discovered Pt severely orthopneic, has to sleep on many pillows. Becomes dyspneic on exam at <45 degree head-up Exam: HEENT: slightly plethoric, some head/neck swelling. Airway: MP 2, good mouth opening, TM distance and prognath Resp: Bilateral crackles R>L, wheezes primarily on right CV: RRR, no m/r/g, strong radial pulses Abd: soft, NT Neuro: Intact During exam, pt experienced several long bouts of coughing that seemed to make not just her lips, but her entire head and neck blue. Problems Anterior mediastinal mass With SVC obstruction, branch PA occlusion, and some tracheal and mainstem bronchus compression Resulting in: SVC Syndrome Dyspnea and orthopnea WPW I’m alone and far away from help SVC Syndrome Mediastinal tumors are the primary natural cause of SVCS in children and adolescents 50% of these are primary mediastinal tumors Symptoms are secondary to impaired venous drainage of the head, neck and upper extremities Worsen when supine, improve when upright Can include dyspnea, facial and neck swelling, venous distention of neck and chest, wheezing and stridor SVC Syndrome: Brief Anesthetic Considerations Neuro: Obstructed venous drainage may also lead to increased ICP Important to maintain MAP to ensure CPP Airway: Increased edema may increase risk of difficult intubation Pulm: Positive pressure ventilation, by increasing intrathoracic pressure, may further decrease venous return CV: Preload augmentation may be necessary to ensure adequate ventricular filling and maintenance of CO Access: Obstructed upper extremity venous drainage necessitates lower body intravenous access Anterior Mediastinal Mass: Forces at Work In the supine position, two opposing forces maintain the position of the tumor: Negative Intrathoracic pressure – pulls the tumor up Gravity – pulls tumor down If the intrathoracic pressure is made less negative, gravity will win, and the tumor will compress underlying structures Positive pressure ventilation Cessation of spontaneous respiratory efforts Sitting, lateral decubitus or prone positions direct force of mass towards abdomen, left chest or sternum Instead of aorta, SVC and trachea Anterior Mediastinal Mass: Important Studies EKG, Labs, etc… Echocardiogram Assess presence and degree of vascular or cardiac compression SVC, RA, pulmonary arteries and pulmonary veins susceptible to compression due to low internal pressure Function and pericardial involvement CAT Scan Assess size and position of mass Effect on adjacent structures Anterior Mediastinal Mass: PFTs? Several authors advocate routine measurement of PFTs Dynamic measurement of presence and degree of obstruction Can be done both seated and supine to assess functional changes PFTs do little to help predict intraoperative morbidity and mortality in this population No study to date has predicted perioperative airway complications from spirometry alone prospectively Although, PFTs can help predict postoperative respiratory complications Tracheal compression >50% on CT and Peak Expiratory Flow Rate < 40% [Bechard P et al, Perioperative respiratory complications in adults with anterior mediastinal mass, Anesthesiology 2004] AMM: Basic Anesthetic Considerations Maintain spontaneous ventilation Awake/sedated FOB intubation if ETT necessary Consider a partial left lateral decubitus position Have a rigid bronchoscope ready If tracheal compression occurs despite precautions and/or if ETT unable to be easily advanced in trachea Lower extremity access Have a quick way to flip pt prone Consider CPB In cases of severe vascular compression, cannulate for CPB while pt still awake. The Plan Created a ramp on the CT scanner, ~30degrees Plan to use local and nothing In the words of one of my PICU attendings, Dr. Brad Peterson: “Anesthesia’s a goddamned luxury. If they make it back to complain to you in a couple years, you’ve done a good job.” Placed lower extremity IV Small dose ketamine (0.25mg/kg) and glyco if sedation was necessary I know, I know….. Fentanyl and Midaz would potentially lead to respiratory depression (especially in doses sufficient to allow pt to remain still), and propofol may increase venous capacitance, leading to even poorer venous return. I chose the Devil I knew Prepare for war Epi, code drugs, LMA, etc. What Happened Pt extremely anxious, almost hyperventilating Could not lay on 30 degree ramp without significant dyspnea Anxiety was definitely contributing to difficulties Sat pt up, and explained again, carefully, why I wasn’t giving her any medication Proceeded with 20mg Ketamine, preceded by 0.6mg Glycopyrollate What Happened Pt was still, breathing comfortably with no evidence of obstruction, and laying on ramp. Started coughing Airway free of oral secretions Improved with another 20mg ketamine. And Then..... Pt began coughing again, and did not stop. Sats started to drop. Attempted to assist ventilation with bag and mask and 100% O2 No appreciable help Sats continued to drop..now in 70s and pt still coughing Pts BP, which, up to this point was ~110/60, was dropping to 80/40 And Then...... Attempted to place LMA and deepen anesthesia with more ketamine LMA 4 and 80mg ketamine Ketamine administered with 10mcg EPI, given risk of circulatory collapse LMA did not help, sats in 50% range, BP steady, HR in 130s Copious frank blood began to come from pts nose and mouth LMA insertion easy and atraumatic Most likely secondary to increased venous pressure coupled with acutely elevated and sustained increase in intrathoracic pressure ........... The patient required control of her airway and 100% O2 For oxygenation, ventilation and protection from what seemed to be only upper airway blood But was possibly on the verge of circulatory collapse secondary to mass compression of vasculature Couldn’t paralyze, and didn’t want to give any further narcotics or sedatives Waited until she took a breath in between bouts of coughing, saw where the bubbles were coming from, and slipped an ETT in ........ Frank blood from ETT after placement 100% O2 with GENTLE positive pressure and ~0.5 MAC of Sevoflurane Sats returned, BP required continued boluses of Ephedrine and Epi, plus 1.5L Crystalloid. Biopsies obtained Left intubated, taken to PICU Extubated next day without issue. Pt with no memory of event. What I learned Better safe than sorry a late, non emergent case, with a patient with this many issues, can be put off until there are a lot more hands around Perhaps tried a slight decubitus position as well? Especially in the face of the coughing. Preparation is key