Mediastinium
advertisement
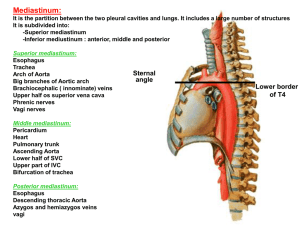
Introduction The mediastinum is the region in the chest between the pleural cavities that contain the heart and other thoracic viscera except the lungs Boundaries Lateral Anterior Posterior Superior Inferior - parietal pleura - sternum - vertebral column and paravertebral gutters -thoracic inlet - diaphragm Mediastinal Anatomy The Mediastinum Normal Mediastinum Anterior mediastinum Everything lying forward of and superior to the heart shadow Boundaries Sternum, first rib, imaginary curved line following the anterior heart border and brachiocephalic vessels from the diaphragm to the thoracic inlet Contents Thymus gland, substernal extension of the thyroid and parathyroid gland and lymphatic tissues Normal Mediastinum Middle mediastinum Dorsal to the anterior mediastinum, extends from the lower edge of the sternum along the diaphragm and then cephalad along the posterior heart border and posterior wall of the trachea Contents Heart, pericardium, aortic arch and its major branches, innominate veins and superior vena cava, pulmonary arteries and hila, trachea, group of lymph nodes, phrenic and upper vagus nerve Normal Mediastinum Posterior Mediastinum Occupies the space between the back of the heart and trachea and the front of the posterior ribs, and paravertebral gutter It extends from the diaphragm cephalad to the first rib Contents Esophagus, descendng aorta, azygos and hemiazygos vein, paravertebral lymph nodes, thoracic duct, lower portion of the vagus nerve and the symphathetic chain Clinical Presentation Asymptomatic mass Incidental discovery – most common 50% of all mediastinal mass are asymptomatic 80% of such mass are benign More than half are malignant if with symptoms Clinical Presentation Effects on Compression or invasion of adjacent tissues Chest pain, from traction on mediastinal mass, tissue invasion, or bone erosion is common Cough, because of extrinsic compression of the trachea or bronchi, or erosion into the airway itself Hemoptysis, hoarseness or stridor Pleural effusion, invasion or irritation of pleural space Dysphagia, invasion or direct invasioin of the esophagus Pericarditis or pericardial tamponade Right ventricular outflow obstruction and cor pulmonale Clinical Presentation Superior vena cava Vulnerable to extrinsic compression and obstruction because it is thin walled and its intravascular pressure is low, and relatively confined by lymph nodes and other rigid structures Superior vena cava syndrome Results from the increase venous pressure in the upper thorax , head and neck characterized by dilation of the collateral veins in the upper portion of the head and thorax and edema oand phlethora of the face, neck and upper torso, suffusion and edema of the conjunctiva and cerebral symptoms such as headache, disturbance of consciousness and visual distortion Bronchogenic carcinoma and lymphoma are the most common etiologies Clinical Presentation Hoarseness, invading or compressing the nerves Horners syndrome, involvement of the sympathetic ganglia Dyspnea, from phrenic nerve involvement causing diaphragmatic paralysis Tachycardia, secondary to vagus nerve involvement Clinical manifestations of spinal cord compression Clinical Presentation Systemic symptoms and syndromes Fever, anorexia, weight loss and other non specific symptoms of malignancy and granulomatous inflammation Pneumomediastinum Air in the mediastinum is a common complication of mechanical ventilation is also commonly encountered in some conditions Pain is the most common symptom Results from stretching of the mediastinal tissues Substernal and aggravated by breathing and changing position Dyspnea, dysphagia, subcutaneous crepitation Mediastinitis Acute inflammation of the mediastinum Substernal chest pain, chills, high fever, prostration Techniques for visualizing the mediastinum and its content Radiographic technique Standard postero antero and lateral views Most mediastinal tumors are discovered Fluoroscopy and tomography Computed tomography Can identify normal anatomic variations and fluid filled cyst Site of the origin of the mass can be better identified 100% specificity for the CT appearance of teratomas, thymolipoma, omental fat herniation Overall accuracy for predicting mediastinal mass is only 48% Computed tomography Limitation Horizontal oriented structures and boundaries are difficult to evaluate Abnormalities in the aortopulmonary window area and the subcarinal area CT has become the initial imaging procedure of choice for evaluation of mediastinum in patients with primary mediastinal mass or with lung cancer Magnetic Resonance Imaging Assesses tissue by measuring the radiofrequency induced nuclear resonance instead of measuring the attenuation of transmitted ionizing radiation Coronal and sagittal planes are better viewed, vertical structures and boundaries are better evaluated Superior sulcus tumors, lesions invading the medistinum, chest wall and diaphragm And possible invasion of the brachial plexus, and for evaluating vertebral invasion Magnetic Resonance Imaging Limitations Distinguish poorly between hilar mass and adjacent collapsed or consolidated lung Cannot distinguish between a benign and a malignant causes for lymph node enlargement Ultrasonography For cystic nature of mediatinal mass Useful in guiding endoscopic biopsy technique Radionuclide imaging Rely on the localization of markers based on specific metabolic or immunologic properties of the target tissue Potential ability to diagnose and stage a malignancy and identify distant metastasis Planar imaging with gallium 67 and thallium-201 POSITRON EMISSION TOMOGRAPHY The technique is not infallible because certain non- neoplastic processes, including granulomatous and other inflammatory diseases as well as infections, may also demonstrate positive PET imaging Size limitations are also an issue, with the lower limit of resolution of the study being approximately 7 to 8 mm depending on the intensity of uptake of the isotope in abnormal cells One should not rely on a negative PET finding for lesions less than 1 cm on CT scan ENDOSCOPIC ULTRASOUND Superior ability to sample the posterior mediastinum through the esophageal wall For patients with lung cancer and posterior mediastinal adenopathy seen on chest CT scan EUS has a sensitivity and specificity of 90% and 100%, respectively. Mediastinoscopy Allows direct inspection and biopsy of lymph nodes or other masses on the superior portion of the anterior mediastinum MEDIASTINOSCOPY Mediastinoscopy remains the gold standard for invasively staging the mediastinum If there is mediastinal adenopathy on CT, often a surgical mediastinal procedure is performed Mediastinoscopy is most often used to sample lymph nodes in the Paratracheal (station 4) Anterior subcarinal (station 7) The subcarinal area is more difficult to sample and thus has a lower yield MEDIASTINOSCOPY