VARICOCELE
advertisement
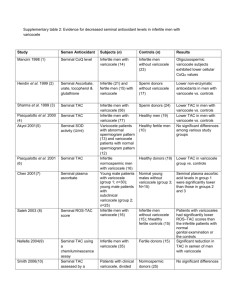
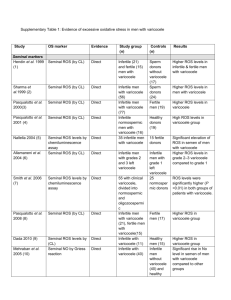
Varicocele UROLOGY Presented by Dr.Hassan sabbagh Urology department Al-Mowassat Hospital 20/2/2014 Definition A varicocele is a dilatation of the pampiniform venous plexus and the internal spermatic vein . Varicocele is a well-recognized cause of decreased testicular function.. occurs in approximately 15-20% of all males and in 40% of infertile males. varicocele are the most common cause of poor sperm production and decreased semen quality. Varicoceles are easy to identify and to surgically correct. Etiology Varicoceles are much more common (approximately 80-90%) in the left testicle than in the right because of several anatomic factors, including: 1) the angle at which the left testicular vein enters the left renal vein. 2) the lack of effective antireflux valves at the juncture of the testicular vein and renal vein. 3) the increased renal vein pressure due to its compression between the superior mesenteric artery and the aorta( the nutcracker phenomenon) 4) Increased length of the left testicular vein: The left vein is 8-10 cm longer than the right testicular vein 80% of men with a left clinical varicocele had bilateral varicoceles revealed by noninvasive radiologic testing. Lt.spermatic vein pressure=10mm Hg and ends in lt.renal vein which pressure =10mm .Hg.so any strain can be detected by increase intra abdominal pressure by valsalva m . In Rt.side :Rt.spermatic vein pressure =10 mm Hg and ends in IVC which pressure =ZERO .So due to increase intra abdominal pressure not increasing pressure Over Rt.spermatic vein. Right side varicocele : We shoud consider possible retroperitoneal pathology (eg,renal cell carcinoma) As the cause of spermayic vein compression. Investigate further with approprite ultrasonography Or Ct scanning befor repairing the varicocele. Pathophysiology Varicocele is associated with a progressive and durationdependent decline in testicular function. 1.) Elevated intrascrotal temperature resulting in reductions in testosterone synthesis by Leydig cells,/ injury to germinal cell membranes,/ altered protein metabolism/& reduced Sertoli cell function/. 2.) The free reflux of renal and adrenal metabolites from the left renal vein are directly gonadotoxic . 3.) Impaired venous drainage results in hypoxia, poor clearance of gonadotoxins, and elevated levels of oxidative stress. Pathophysiology The increased hydrostatic pressure in the intrascrotal veins enhances the physiological countercurrent exchange from these veins to the testicular artery. Presentation usually asymptomatic and often seeks an evaluation for infertility after failed attempts at conception. He may also report scrotal pain or heaviness. An obvious varicocele is often described as feeling like a bag of worms. The presence of a varicocele does not mean that surgical correction is a necessity. Grading • Despite having a congenital background it is not diagnosed before the age of 10 years. Grade I: Small, detectable only during the Valsalva maneuver. Grade II: Moderate, can be palpated without Valsalva. Grade III: Large, visible through the scrotal skin & classically described as feeling like a “bag of worms”, & decompresses in supine position. Sub-Clinical Varicoceles are those not detected clinically but diagnosed only detected by ultrasonography with or without doppler, radionucleotide scans, thermography & venography. Diagnosis and Investigations Physical Examination The physical examination has been the Varicocele method most commonly used . Testicular size and volume should be assessed. Varicoceles diagnosed by physical examination are considered “clinical” and they are classified according to their size. Doppler US Although clinical varicoceles do not require h confirmation with ultrasound examination, color Doppler ultrasound may be required when the clinical examination is difficult. Demonstration of reversal of venous blood flow with the Valsalva maneuver or spermatic vein diameters of 3 mm or greater support the diagnosis of varicocele. color Doppler ultrasound has more than 90% sensitivity and specificity. Venography Venography of the internal spermatic veins has been used to diagnose and treat varicoceles. nearly 100% (Most Sensitive) of clinical varicocele patients will demonstrate reflux on venographic examination. left internal spermatic vein reflux has been reported in up to 70% of patients without a palpable varicocele. (High false positive results & Limited Specificity) Semen Analaysis Clinical Treatment for Varicocele There are few well-designed studies about medical treatment for varicocele. The use of carnitine combined with nonsteroidal antiinflammatory drugs for 6 months in patients with clinical varicocele and infertility was not able to solve improve semen parameters or achieve a higher pregnancy rate. Clomiphene citrate has been shown to have no effect on sperm concentration and motility in patients with subclinical varicocele. There is a benefit of antioxidants in patients with varicocele. Indications for Intervention Not everyone with a varicocele needs to have it corrected. This determination should be made on a caseby- case basis. 1) Large varicoceles producing clinical symptoms such as dull hemiscrotal discomfort or sense of heaviness. 2). The couple has known infertility with the female partner has normal fertility. 3). The male partner has one or more abnormal semen parameters or abnormal results from sperm function tests. 4). Adolescent males with unilateral or bilateral clinical varicoceles & ipsilateral testicular hypotrophy (20% or 3ml volume decrement from the contralateral testis) 5) cosmetic appearance, particularly when the varicocele is extremely large. Varicocoeles in childhood Varicocoeles can be demonstrated in 6% of 10- year-old boys and 15% of 13 year olds. spermatogonia, seminiferous tubal atrophy, endothelial cell proliferation and Leydig cell abnormalities. When foundin patients under 18 years of age the changes are potentially reversible Indications for treatment The presence of symptoms is generally accepted as an indication for surgical intervention, as is impairment of testicular growth. ‘prophylactic’ intervention in the case of the larger, grade III, lesions, particularly if there is testicular asymmetry with a discrepancy in testicular volume of >20%. Recovery of testicular volume in adolescent patients, so called “catch-up growth,” has been reported to occur in up to 80% of boys with grade II or III varicoceles. Methods Of Surgical Repair Scrotal Approach Retroperitoneal approaches (Open or Laparoscopic) Inguinal Approach Sub-Inguinal Approach Radiographic Occlusion Techniques (Embolization) Scrotal Approach The very 1st approach for varicocele repair employed in the early 1900s. Involves mass ligation & Excision of the varicosed veins. Not preferred practically due to the high incidence of testicular artery injury with subsequent impairment of the testicular blood supply, testicular atrophy & more impaired spermatogenesis & fertility. Retroperitoneal(Palomo)Approach Incision at the level of the internal ring near to the Anterior Superior Iliac Spine. Exposure of the Internal Spermatic Artery & Vein retroperitoneaelly near the ureter where only one or two large veins are present & the testicular artery is not yet branched & so easy to separate. A disadvantage of a retroperitoneal approach is the high incidence of varicocele recurrence, especially in children and adolescents, when the testicular artery is intentionally preserved. Causes of recurrence 1) preservation of the periarterial plexus of fine veins along with the artery. These veins have been shown to communicate with larger internal spermatic veins. 2)presence of parallel inguinal or retroperitoneal collaterals, which may exit the testis and bypass the ligated retroperitoneal veins, rejoining the internal spermatic vein proximal to the site of ligation. 3)Dilated cremasteric veins, another cause of varicocele recurrence, cannot be identified with a retroperitoneal approach The incidence of recurrence appears to be higher in children, with rates reported between 15% -45% in adolescents. Recurrence is prevented by intentional artery ligation, However it may cause testicular atrophy & subsequent azoospermia. Laparoscopic Approach It is an essence retroperitoneal approach with similar advantages & disadvantages, including rate of recurrence. The internal spermatic veins are ligated with the laparoscope at the same level as the retroperitoneal approach with preservation of the testicular artery. The potential complications of laparoscopic varicocelectomy (injury to bowel, vessels or viscera, air embolism, peritonitis). Laparoscopic Approach is a reasonable alternative for the repair of bilateral varicoceles. The Inguinal Approach can be used in almost any patient It allows for mobilization of the cord, identification of any large veins within the cremasteric muscle. identification of veins perforating the posterior inguinal canal that might be contributing to the varicocele. Conventional inguinal operations are associated with an incidence of postoperative hydrocele formation varying from 3% to 15%. Subinguinal Approach The incision is made just below the level of the external inguinal ring The advantage of this technique is that it requires a small incision with no abdominal muscle or fascia cut. At the subinguinal level, however, significantly more veins are encountered. identification and preservation of testicular artey more difficult it is best to use in men with a history of any prior inguinal surgery. Radiographic Occlusion Techniques Does not prevent recurrence (4% to 11%) but allows visualization of all collaterals difficult to be seen with the 2D view. Drawbacks: 1) Take 1-3 hours to perform compared with 25 to 45 minutes required for surgical repair. 2) Femoral vein perforation or thrombosis. 3) Anaphylaxis to radiographic medium. 4) Recurrence with large varicoceles & with Failure to cannulate small collaterals. 5) Migration of the balloon or coil into the renal vein, resulting in loss of a kidney, pulmonary embolization. Complications of Varicocelectomy Hydrocele the most common complication reported after nonmicroscopic varicocelectomy. The incidence of this complication varies from 3% to 33%, with an average incidence of about 7%. hydrocele formation after varicocelectomy is due to lymphatic obstruction. Use of magnification to identify and preserve lymphatics can virtually eliminate the risk of hydrocele formation. Testicular Artery Injury The diameter of the testicular artery in humans is 1.0 to 1.5 mm The testicular artery supplies 2/3 of the testicular blood supply, and the vasal and cremasteric arteries supply the 1/3. Injury or ligation of the testicular artery carries with it the risk of testicular atrophy and/or impaired spermatogenesis. (which is less likely to occur in children due to compensatory neovascularization). The Use of Magnification & Micro-Doppler helps good identification & Preservation of the testicular artery. Varicocele Recurrence The incidence of recurrence after varicocele repair varies from 0.6% to 45%. Recurrence is mostly associated with: 1). Pediatric Varicocele 2). Non-Magnified Operations 3). Retro-peritoneal approaches (that misses the parallel inguinal collaterals. Results Varicocelectomy results in significant improvement in semen analysis in 60% to 80% of men. Reported pregnancy rates after varicocelectomy vary from 20% to 60%. Microsurgical varicocelectomy results in return of sperm to the ejaculate in up to 60% of azoospermic men with palpable varicoceles. Repair of large varicoceles results in a significantly greater improvement in semen quality than repair of small varicoceles. pregnancy rate 1500 microsurgical operations varicocelectomy control group • 43% of couples were pregnant at 1 year. • 10% in the control group. • 69% at 2 years • 13%at 2 years these Table show improvements in seminal parameters with varicocele repair and specific functional testing to include sperm penetration assay, sperm DNA fragmentation levels and oxidative stress levels. varicocele repair reported mean increases in: sperm density of 9.7 million/mL, motility increases of 9.9%, and WHO sperm morphology improvement by 3% The vast majority of azoospermic patients with return of sperm postvaricocele treatment will still require advanced ART such as in-vitro fertilization to obtain conception. Spontaneous pregnancy rates after varicocele treatment average between 30% and 50% with pregnancies occurring at an average of 8 months after treatment. CONCLUSION Varicocele is one of the most common cause of male infertility. The presence of varicocele must be detected in all patients with abnormal Semen quality,including azoospermia. Varicocelectomy results in significant improvement in semen analysis in 60% to 80% of men and Spontaneous pregnancy rates after varicocele treatment average between 30% and 50%. Comparisons of surgical approaches for varicocelectomy By Dr. Hassan sabbagh We compare the outcomes of three microsurgical techniques: inguinal high ligation (IHL) =40 patient Retroperitoneal high ligation(RHL) =40 patient Low ligation(LL) =40 Patient we compared the operation time, post operative complication Recurrence rate. The result was……………. Operation time 60 50 40 30 OperationTime 20 10 0 Inguinal Retro High ligation Low Ligation 18% 16% 14% 7.50% 12% Epididymitis Hydrocele 10% 8% 6% 5% 10% 4% 5% 2% 2.50% 2.50% 0% Inguinal Retro-Peritoneal HL Low Ligation Recurrence rate 5% 5% 4% 4% 3% 3% Recurrance 2% 2% 1% 1% 0% Inguinal Retroperitoneal Hl Recurrence rates inguinal 5% (2 cases) Retroperitoneal HL 2.5% (1case) Low ligation LL (none case) Low Ligation Retroper itoneal HL 2.5% Inguinal 5% Low ligation 0% Recurrence rates Conclusion As a microsurgical approach to the treatment Of varicocele ,low ligation is better than inguinal High ligation and retroperitoneal high ligation in improving Recurrence rate and seminal parameters of the patients. Objective: to evaluate the post operative complications Of microscopic and conventional palomo varicocelectomy Microscopic palomo varicocelectomy Group A(n=130) Conventional palomo Group B (N=130) The Postoperative complications and recurrence were compered Between the tow groups. The result after 1 year of follow up were………….. 0.9 0.8 0.7 0.6 testicular atrophy testicular pain 0.5 0.4 0.3 0.2 0.1 0 microscopic conventional palomo Testicular atrophy rates 0.7% vs 3.1% Testicular pain rates 90.7% vs 67.7% Group A (microscopic)=130 p Group B (conventional palomo)=130 p Recurrence rates 6.00% 5.00% 4.00% 3.00% recurrence 2.00% 1.00% 0.00% microscopic Recurrence rates Group A 5.3% vs Group B 3.8% conventional palomo Objective: to compare the outcomes of the different surgical Techniques used in varicocelectomy wich include: Inguinal approach (40 p ) Laparoscopic approach (40 p) Subinguinal microscopic approach (40 p) The assessment included postoperative complications ,and Postoperative semen analysis and pregnancy rate after 18 mon. The result was………….. Postoperative complications 20% 18% 16% 14% 12% hydrocele recurrence 10% 8% 6% 4% 2% 0% inguinal laparoscopic microscopic subinguinal Inguinal: hydrocele 13% +13% recurrence. Laparoscopic: 20% +18% . Microscopic subinguinal : 0% +0.5% . Laparoscopic 18% Inguinal 13% Microscopic subinguinal 0.5% Recurrence Improvement of sperm motility and concentration 78% 76% 74% 72% 70% sperm mobility and concentration 68% 66% 64% 62% 60% 58% inguinal laparoscopic microscopic subinguinal Inguinal: 65% Laparoscopic:.67% Microscopic subinguinal : 76% Pregnancy rate after 1 year 40% 35% 30% 25% 20% pregnancy rate 15% 10% 5% 0% inguinal laparoscopic microscopic sub inguinal Inguinal: 28% Laparoscopic:. 30% Microscopic subinguinal : 40% Conclusions The findings of our study have demonstrated That , compared with open inguinal ,laparoscopic, and microscopic Sub inguinal . Sub inguinal microsurgical varicocelectomy offers The best outcomes. Varicocele management A comparison of Palomo versus Inguinal approach 2009 Patient and Methods: 52 patients were included in study.Randomly 26 patients were Operated In each group i.e inguinal and palomo. All patients were followed at 3 and 6 months and 1 year. The results were ………………………… Inguinal approach versus palomo 12.00% 10.00% 8.00% wound haematoma wound infection hydrocele recurrence 6.00% 4.00% 2.00% 0.00% Inguinal approach Palomo approach Inguinal approach: 2(7.7%) +1(3.9%) +1 (3.9% ) +1 (3.9%) Palomo approach: 1(3.9%) + 0 % +0 % +3(11.6%) Conclusion It is concluded the palomo operation Is better than inguinal approach for varicocelectomy. There is decreased complication rate and better Patient satisfaction. However recurrence is less in inguinal approach. Both Procedures improve fertility.however choice of procedures seems to be More of surgeon,s training and personal liking Than considering benefits and draw backs of both procedures. Objectives: The aim of this study was to evaluate the outcome of varicocelectomy using a modified microsurgical method, specifically a loupe-assisted method, and its effects on sperm parameters in infertile men. Patients and Methods: This study was performed in 40 patients who presented with varicocele. All patients had at least a 1-year history of infertility with abnormal semen parameters and varicocele proven by physical examination 20 patients were treated by a sub-inguinal approach assisted by loupe magnification (Group A) 20 patients were treated by the same approach but without magnification (Group B). To facilitate the procedure, an ×3.0 loupe was used during the spermatic cord dissection. The Results were………….. Post-Operative Complications Group A, No.(%) (n Group B, No.(%) (n = 20) = 20) Scrotal hematoma 1 (5) 2 (10) Wound infection 2 (10) 2 (10) Hydrocele - 3 (15) Recurrence - 2 (10) Scrotal edema - 2 (10) Complication Conclusions: Loupe-assisted sub- inguinal varicocelectomy is a safe, simple, and effective method for the treatment of sub-fertile men, especially in medical facilities without microscopic equipment, and permits significant improvement in sperm parameters.