Urinary System
Urinary System
•
•
Essential to life
Every head to toe
assessment must
include…
–
urinary tract
function
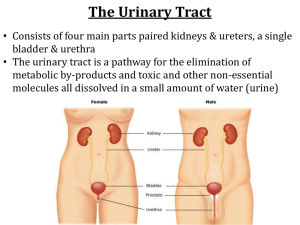
Anatomy: Kidney
• Kidneys
– Vascular
– Shape
• Bean
– Color
• Brown-red
– How many / #
•2
Anatomy: Kidney
•
3 areas
–
–
–
Cortex
Medulla
Cortex
Medulla
Renal Pelvis
Renal Pelvis
Kidney: Cortex
• Contains
– Nephrons
• Functional unit of the
kidneys
• Glomeruli / glomerulus
• Filters blood
• Creates urine
Kidney: Medulla
• Function
– Drain urine from
the Nephrons to
the renal pelvis
Kidney: Renal Pelvis
• Ureter
• Renal artery
• Renal Vein
Anatomy: Nephrons
• FYI
– Functional unit*
– 1 million Nephrons in
ea. Kidney
– Adequate renal
function with 1
kidney
Urine flow
•
•
•
•
Nephrons
Medulla (pyramids)
renal pelvis
ureter
Anatomy: Ureters
•
•
•
•
Long narrow
muscular tube
Moves urine via
peristaltic waves
Extends from renal
pelvis bladder
Two
Anatomy: Bladder
BLADDER
• Description
–
–
•
Location
–
•
Muscular
hollow sac
Behind pubic bone
Function
–
Reservoir for urine
Anatomy: Bladder
• Normal capacity
– 300-500 ml of urine
Anatomy: Urethra
•
Carries urine from
the bladder & expels
it from the body
Physiology of the Urinary System
•
Function of the
kidneys
–
–
Urine formation
Excretion of waste
products
Regulation of
–
•
•
•
•
Electrolytes
Acid-base control
RBC production
Ca+ & Ph
– Control
• water balance
• blood pressure
– Renal clearance
– Synthesis of Vit. D
Physiology of the Urinary System
•
Urine formation
–
The nephrons form
urine through a
complex process
Anatomy: Nephrons
• Nephron
– Glomerulus
– Bowman’s capsule
• Proximal convoluted
tubule
• Loops of Henle
• Distal convoluted
tubule
Regulation of water excretion
•
The amt. of urine formed is r/t
the amt. of fluid intake
–
–
h fluid intake
volume urine
•
h
•
Characteristic
–
–
–
Dilute
i fluid intake
volume of urine
•
•
i
Characteristic
–
Concentrated
Excretion of waste products
•
Urea, (waste product)
–
Blood Urea Nitrogen
•
•
h BUN = renal dysfunction
Creatinine
–
–
The creatinine clearance compares the level of
creatinine in urine with the levels in the blood
i Creatinine clearance = renal dysfunction
Excretion of waste products
• Primary means of ridding the
body of Drug metabolism
Small Group Question
1. Describe the flow of urine from formation to
excretion
2. What is the functional unit of the urinary
system? What does it do?
3. Increased or decreased fluid intake has what
effect on volume of urine and its
characteristics
4. What two main waist products do the
kidneys rid the body of?
Assessment:
• Urine
– Color
– Odor
– Amount
• Difficulty urinating
• Fluid intake
• Painful urination
– dysuria
Assessment
• Urinating at night
– Nocturia
• Blood in the urine
– Hematuria
• Cloudy urine
– Pyuria
• Discharge?
Assessment
• Pain
– Abd
– Suprapubic
– Flank
Assessment: Health history
•
•
•
•
•
•
Symptoms
Associated symptoms
Hx of UTI’s
Meds
Smoking or Alcohol
Females
– Pg
Physical Assessment
• Urine sample
– Clean-catch
• V/S
• Skin
– Color
– Moisture
– Edema
• Palpate abd
• Percuss kidney for
tenderness
Physical Exam
•
Abdomen,
supropubic region,
genitalia and lower
back, the lower
extremities
Physical Exam
• Palpation of bladder
– Performed after voiding
if suspect urinary
retention
Urinalysis: normal
• Color
– Light straw – amber
– Clear
• Specific gravity
– 1.005 – 1.030
• pH
– 4.5 – 8.0
• Protein
– Neg - trace
Urinalysis: normal
• Glucose
– -
• Ketones
– -
• RBC
– 1-2
• WBC
– 3-4
• Casts
– -
• Bacteria
– -
Specific Gravity
•
•
The weight of urine
Related to the level of hydration.
–
–
h fluid intake h H20 excretion i specific gravity
i fluid intake i H20 excretion h specific gravity
Diagnostic Evaluation:
Urine Culture and Sensitivity
•
•
•
ID microorganism(s)
Sensitivity report
Time
–
2-3 days (48-72 hours)
Diagnostic Evaluation:
Clean-catch or Clean-voided specimen
• Clean-voided
– uncontaminated by skin flora.
– Female
• Cleanse: front to back
– Male
• Cleanse: tip of the penis downward
• Collect a "clean-catch"
– Start to void
– Midstream catch
– Collect 1 to 2 oz of urine
Diagnostic Evaluation:
Sterile urine specimens
•
Safety
–
–
•
Standard precautions
Biohazard bag for transport
Collection
–
Indwelling Foley Catheter
•
•
–
Not from the drainage bag
Aspiration port
Catheter – straight cath
–
A small amount of urine is allowed to run out of the catheter into
a basin, then the urine is allowed to run into a sterile specimen
bottle.
I&O
Intake
•
Oral liquids
–
–
–
–
•
Milk
Tea
Juice
Broth
Liquid at room temp
–
–
•
•
Output
Ice cream
Jello
NGT/GT
IV
•
•
•
•
Urine
GI suction
Emesis
Drainage
– Chest tubes
– Wound tubes
• Healthy person
• Fluid output =
• Fluid input
• If the client takes in
more fluid than they
excrete
– edema
S&S Edema
• Weight
–h
• Swelling
–
–
–
–
Feet
Ankles
Face
Fingers
• Urine output
– i
• Fluid pooling
– Lungs
– Abd
• Ascites
• Pitted edema is tested by pressing & holding
your finger into the swollen tissue over a bony
area for 5 seconds. If there is an indentation left
behind when you remove your finger it is pitted
edema.
• To classify the pitted edema you measure the
depth of pitting & compare the measurement to
the following scale;
• +1 = 2mm of pitting
• +2 = 4mm of pitting
• +3 = 6mm of pitting
• +4 = 8mm of pitting
What is the nursing diagnosis for a
client with edema?
• Fluid Volume Excess
• If a client excretes more
fluid than they take in
– dehydration
Dehydration S&S
• Thirst
• Constipation
• Urine output
–i
• BP
– i
• Pulse
– Weak
–h
• Mentation
– Confused
– Lethargy
• Skin
– Dry
• Mucus membranes
– Dry
• Weight
–i
1. Describe the nursing assessment of a client who
is complaining of voiding issues?
2. What dx test do you expect the doctor to order
for a client with renal failure
3. What does a UA measure & what should not be
found in the blood.
4. Increased & decreased fluid intake have what
effect on specific gravity
5. Describe how to get a clean catch and a sterile
urine specimen?
Cystitis
• Inflammation of the
urinary tract
– Bladder
– UTI
• Etiology
– Bacteria
Cystitis: S&S
•
•
•
•
•
•
•
Dysuria
Frequency
Urgency
Nocturia
Pyuria
Hematuria
Lower abd discomfort
Gerontologic considerations
•
•
•
•
Few S&S
Fatigue
Alt cognitive function
drop in temp
Defense Mechanism
• Who is more likely to get a UTI
A. Male
B. Female
• Why?
– Shorter urethra
Pyelonephritis
• Inflammation of the
renal pelvis &
parenchyma
• Etiology
– Bacteria
• E-coli
Pyelonephritis: S&S
• S&S of Cystitis
–+
•
•
•
•
Flank pain
Vomiting / diarrhea
Fever / chills
Malaise
Assessment & Dx findings
• Urinalysis
– UA
• Culture
Medical management/
pharmacological therapy
• Antibiotic
• Urinary analgesic
Nursing Process: UTI
• Assessment
–
–
–
–
S&S
Voiding patterns
Sexual intercourse
Urine
Nursing: health promotion
• Fluid intake
–h
• Void when you feel the
need
– Q3-4 hours
• Female
– Clean front to back
• Void after intercourse
• Avoid
– bubble bath
– Feminine hygiene
– Douching
• Cotton underwear
• Shower not bath
Nrs Dx: Pain
•
•
•
Assess pain
Admin. Analgesics, antibiotics per order
Teach non-Rx
– Heating pad
– Warm showers
• Cranberry juice
• Vitamin C
• Avoid excess milk, fruit juice
1. What are the S&S of cystitis?
2. Differentiate with cystitis & Pyelonephritis
3. What are the gerontological considerations
for a client with a UTI?
4. What would you teach a client about
preventing further UTI’s
Glomerulonephritis
• Inflammation of the
glomerulus
– Damage
• Blood
• Protein
• escapes into tubule
Glomerulonephritis
• Etiology
– Acute
• Bacterial infection
– Chronic
• Diabetes
• Lupus
Nephrotic syndrome
•
Group of symptoms (glomerulonephritis)
•
•
•
•
Protein in the urine
i serum albumin
Edema
h serum cholesterol
Nephrotic syndrome
–
Clinical Manifestation
•
•
•
•
•
#1 – edema
Malaise
H/A
Irritability
Fatigue
Glomerulonephritis
•
Assessment and diagnostic findings
–
–
–
–
–
Edema
Proteinuria
Hyperlipidemia
Hypoalbuminemia
Azotemia
•
Increased waste product in the blood
–
(Urea, Creatinine etc.)
Glomerulonephritis
• Complications
– Renal Failure
– Embolism
Glomerulonephritis
• Medical Management
– Edema
• Diuretic
– Inflammation
• Glucocortioids
• NSAID
– Infection
• Antibiotics
– Diet
• Sodium
– i
• protein
– h
– Azotemia i
• Fat
– i
Glomerulonephritis
• Nursing Management - Edema
– qD weight
– I&O
– Abd. Girth
– Clean skin
– Diet per order
Kidney stones /Renal Calculi
• Risk factors
–
–
–
–
Dehydration
Urinary stasis
Infection
Immobility
Renal calculi or nephrolithiasis
• Clinical Manifestations
– Pain
• Abd / flank
• Severe
• N&V
– Hematuria
Renal calculi or nephrolithiasis
•
Assessment and
diagnostic findings
–
–
–
–
UA
X-ray
CT-scan/MRI
Cystoscopy
Renal calculi
• Cystoscopy
– Lighted scope to inspect
bladder
– Gen anesthesia
Renal calculi
•
Medical management
–
Pain relief
•
•
–
–
Opioid analgesic
NSAIDs
Diuretics?
Antibiotics?
Renal calculi
•
Medical
management
–
Diet
•
•
•
Fluids
i protein
i Sodium
Renal calculi or nephrolithiasis
•
Surgical
Management
–
–
If > 4mm will not
pass through ureter
If not pass
spontaneously or if
complications
surgery
Nrs Dx: Acute Pain / Deficient knowledge to
prevent recurrence of renal stone
• Admin Meds
– opioid agents
– NSAIDS
• Position of comfort
• Amb.
• Heat to flank
• Fluids
–h
•
•
•
•
Assess urine
I&O
Strain urine – gauze
Avoid dehydration
Small Group Questions
1. What are the classic clinical manifestations fro a
client with Glomerulonephritis
2. What causes Glomerulonephritis
3. What are the medical interventions for a client
with Glomerulonephritis
4. What are the specific nursing interventions of
this client
5. What are the S&S of renal calculi
6. How is a renal calculi treated?
Cancer of the urinary tract
•
Pathophysiology
–
Most common site
•
–
Bladder
Carcinogen
•
–
–
#1 Tobacco
Metastasize early
1/3 have metastasis at time of diagnosis
Cancer of the urinary tract
• Clinical Manifestations
– Initial
• Painless hematuria
– Late
• Frequency
• Dysuria
Cancer of the urinary tract
• Medical treatment
– Goal:
• Eradicate before metastasis
– Surgery
» Cystectomy
» Nephrorectomy
• Radiation
• Chemotherapy
Renal Failure
• Kidneys unable to
remove accumulated
waste products from
the blood
– Acute
– End-stage
What is the medical term for accumulation of
waste product in the blood?
• Azotemia
Acute Renal Failure
• Abrupt onset
• Often reversible
• Etiology
– Trauma
– Infection
Acute Renal Failure: S&S
• Oliguria
– Urine < 400 mL/day
• BUN
–h
• GFR
–i
• Azotemia
– Confusion
– Na+ & H2O retention
• Edema
• HTN
– Hyperkalemia
End Stage Renal Failure
• Gradual kidney
destruction
End Stage Renal Failure: S&S
• Uremia
–
–
–
–
–
(Urine in the blood)
N/V
Weakness
Fatigue
Confusion
Renal Failure: Tx
• No nephrotoxic drugs
– NSAID’s
• Antihypertensives
• Diuretics
• Fluid
– Restriction
• Sodium
– Restriction
Dialysis: Overview
•
Purpose
–
•
Remove fluids and waste products from the
body
Definition
–
•
Mechanical means of removing waste from the
blood
Types:
–
–
Hemodialysis
Peritoneal dialysis
Dialysis: Process
• Process
– Diffusion and osmosis across a semi permeable
membrane into a dialysate solution
• prescribed specific to the individual clients needs
Dialysis: process
• Diffusion
– Toxins & wastes
are removed by
diffusion
• Osmosis
– Excess water is removed
by osmosis
Hemodialysis
•
A machine with an
artificial
semipermeable
membrane used for
the filtration of the
blood.
Hemodialysis
– The clients blood is
circulated past the
semi permeable
membrane
– Excess fluids are
removed by osmosis
Hemodialysis
• Waste products are
removed from the
blood by diffusion
Hemodialysis
• Frequency
– 2-3 times a week
– Total
• 9-12 hours
Peritoneal Dialysis
•
Uses the peritoneal
lining of the
abdominal cavity
Peritoneal Dialysis
– A catheter is placed
by the MD into
peritoneal space
Peritoneal Dialysis
• Complication
– INFECTION
• Usually 4 x day –
7day/wk