File
advertisement

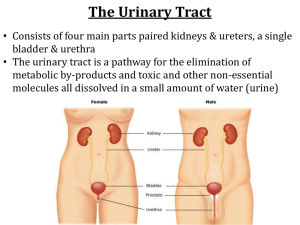
GENITOURINARY SYSTEM Michelle Gardner NUR-224 URINARY SYSTEM ASSESSMENT OF THE URINARY SYSTEM Subjective Data a. Good communication skills b. Avoid medical terminology c. Anxiety/embarrassment – “forget/deny”-- ASSESSMENT DATA Past Health History a. Presence/history of diseases r/t urologic problems – DM, HTN b. Neurologic conditions – back injury, stroke, trauma c. Urinary problems – BPH, renal calculi, cancer, infection ASSESSMENT DATA Medications a. b. c. d. Prescription / OTC / Herbs Nephrotoxic medications -- antibiotics Quantity & character of urine output – diuretic, anticholinergic, antihistamine Change in color – Pyridium, Macrodantin ASSESSMENT DATA Surgery a. Previous hospitalizations r/t urologic disease b. Pelvic surgeries c. Urinary instrumentation d. Urinary problems during past pregnancies e. Radiation/chemotherapy ASSESSMENT DATA Pain Changes in voiding Affects of aging on the urinary system a. Decrease muscle tone b. Decrease bladder capacity c. Prostate enlargement d. Changes in metabolism BLOOD CHEMISTRIES Blood Chemistries Serum Creatinine: 0.6 – 1.2mg/dl o End product of muscle & protein metabolism o Excellent indicator of kidney function o Renal disease results in increase creatinine BLOOD CHEMISTRIES o o BUN/Blood Urea Nitrogen: 7-18mg/dl Used to identify renal problems Nonrenal factors may increase BUN a. Fever b. Dehydration c. High protein diet d. Athletic activity e. Drugs and vitamins (acetaminophen, ibuprofen, vitamin D) DIAGNOSTIC STUDIES o o KUB (kidneys, ureters, bladder) X- ray exam of abdomen & pelvis Used to detect abnormalities o o o o Urinary calculi Cysts Tumors Hydronephrosis DIAGNOSTIC STUDIES o o IVP (INTRAVENOUS PYLEOGRAM) Urography Intravenous injection of radiopaque imaging dye X-ray imaging of dye through upper and lower urinary system INTRAVENOUS UROGRAPHY INTRAVENOUS UROGRAPHY o o o o o o Patient preparation: Consent form Cathartic/enema the night before Identify allergies – shellfish, iodine Pre-medicate–antihistamine (Benadryl) NPO 8 hr. before procedure Transitory effects – contrast medium INTRAVENOUS UROGRAPHY o o o o Post-procedure Monitor vital signs Assess for s/s anaphylactic reactions Monitor urine output Force fluids RENAL ANGIOGRAPHY o o o 1. 2. 3. RENAL ANGIOGRAM: Catheter inserted into femoral artery Contrast material injected through the catheter Visualize renal blood vessels Findings : Renal artery stenosis Differentiate renal cysts from tumors Evaluate hypertension RENAL ANGIOGRAPHY o o o o Patient preparation Consent form Cathartic/enema the evening before Assess allergic reaction Mark peripheral pulses RENAL ANGIOGRAPHY o o o o o Post-Procedure Monitor vital signs Pressure dressing over insertion site Assess insertion site Bedrest with affected leg straight Palpate peripheral pulses RENAL BIOPSY o o Done as a needle biopsy with needle insertion into lower lobe of the kidney OR open biopsy via small flank incision Obtain renal tissue to determine type of renal disease Kidneys are vascular organs – hemorrhage/complication RENAL BIOPSY Patient preparation o Consent form signed o NPO status 8 hrs. prior to test o Assess baseline coagulation status o Medications that may alter clotting function RENAL BIOPSY RENAL BIOPSY Post-Procedure o Pressure dressing applied o Check puncture site – swelling/tenderness o Prone position for 30-60 minutes o Monitor vital signs o Observe for gross bleeding o Assess for flank pain, Hgb./Hct. levels o Avoid lifting heavy object/strenuous activity – 7 days UROLOGIC ENDOSCOPIC PROCEDURES o o a. b. c. d. Visualize/inspect the interior of the urethra and bladder with a tubular lighted scope (cystoscope) Used to: Treat bleeding lesions Insert ureteral catheters Remove calculi Obtain biopsy specimens CYSTOSCOPY o o o o Patient preparation Signed consent form NPO prior to the procedure Local topical anesthetic Lithotomy position – leg cramps CYSTOSCOPY o o o o Post-procedure Expected side effects - burning on urination, blood-tinged urine, urinary frequency Encourage increased fluids Warm sitz bath Mild analgesics RENAL CALCULI UROLITHIASIS/ NEPHROLITHIASIS 500,000 people in the U.S. have kidney stone disease Incidence is highest in Southern & Midwest states. Occurs between the 3rd-5th decade of life. Recurrence of stones – 50% of pts. More common in men than in women RENAL CALCULI Risk Factors Family history of stone formation Dehydration increase urine concentrations Excess dietary intake of calcium, oxalate, or proteins Sedentary lifestyle/immobility Genetic predisposition RENAL CALCULI o o o Stones can be found anywhere from kidney to bladder Vary in size Factors that contribute to urolithiasis * supersaturation * nucleation RENAL CALCULI Pathophysiology Concentration of an insoluble salt is high in the urine supersaturation Crystals form from supersaturated urine Growth continues by aggregation to form larger particles – stone formation RENAL CALCULI RENAL CALCULI 1. 2. 3. 4. 4 Major Categories of Stones Calcium Oxalate Uric acid Cystine Calcium Calculi High concentration of calcium in the blood/urine 70-80% of kidney stones are calcium stones Smaller stones maybe trapped in the ureter Seen more in men Calcium Calculi (Oxalate) Risk factors Hypercalciuria/hypercalcemia, immobility, vit.D, urine intoxication, dehydration Management Thiazide diuretics Limit foods that acidify urine Hydration/exercise Uric Acid Stones Uric Acid Calculi Urine concentration of uric acid is high o Common in men Causes: 1. Gout 2. Increased dietary intake of purine 3. Acid urine o 1. 2. 3. Reduce dietary purines– sardines, mussels, organ meats, aged cheese Administer allopurinol (Zyloprim) Reduce urinary concentration of uric acid Struvite Calculi Struvite Calculi (Staghorn) 15-20 % of stones magnesium/ammonium/phosphate Risk Factors UTIs, esp Proteus infections Stones are large fill renal pelvis Management Antibiotics Surgical intervention/lithotripsy Cystine Calculi o o o o o Make up 1-2% of all stones Caused by genetic defect Tend to form in acid urine Stones appear during childhood / adolescence Rare in adults o o Increase hydration Low-protein diet RENAL CALCULI o o o o o Clinical Manifestations: Severe flank pain / renal colic Abdominal pain Hematuria Oliguria/anuria Nausea /Vomiting/Diarrhea RENAL CALCULI Diagnostic Studies: o Urinalysis o 24 hr urinary measurement for calcium, uric acid o X-ray - KUB o Renal Ultrasonography o CT Scan RENAL CALCULI Management Pain management o Opiod analgesics – Morphine o NSAID Toradal o Comfort measures o Increase fluid intake (oral/intravenous) RENAL CALCULI Stones may pass spontaneously Stones larger than 4mm are unlikely to pass through the ureter Chemical analysis of the stone to determine the composition of the stone STRAIN ALL URINE RENAL CALCULI o o o o o o o THERAPUETIC INTERVENTIONS ESWL-Extracorporeal shock-wave lithotripsy Non-invasive procedure External shock-waves break up the stone No damage to surrounding tissue Stones are fragmented into fine sand Fragments are excreted in the urine All urine is strained -- chemical analysis Anesthesia is necessary RENAL CALCULI o o o o o Cystoscopy passed – removes stones located in the ureter close to the bladder Stone removed -- grasping basket, forceps Stent may be placed Foley catheter -- facilitate passage stone fragments Minimal complications RENAL CALCULI After episode of urolithiasis a. Increase fluid intake – 3000ml/day b. High urine output – 2L/day c. Water is the preferred fluid d. Avoid tea, coffee, colas e. Limit foods high in oxalate, calcium, & purines STRAIN ALL URINE BENIGN PROSTATIC HYPERPLASIA (BPH) • Age–related, nonmalignant enlargement of the prostate gland Enlargement of the prostate gland -compress the urethra/bladder This impedes the normal flow of urine Begins at the age of 40 and continues slowly throughout the rest of life Symptoms appear slightly earlier in AfroAmerican men BPH Begins with small layers in the periuretheral gland Prostate enlarges through formation /growth of nodules and enlargement of glandular cells Enlargement compresses against the urethra urologic symptoms Changes occur over a long period of time BPH Clinical Manifestations Difficulty starting urinary stream Urinary frequency Nocturia Leakage or dribbling of urine Urgency BPH Complications Urinary retention Urinary tract infections Bladder stones BPH Diagnostic Studies History & physical exam Urinalysis/ C&S Digital rectal exam (DRE) Prostatic Specific Antigen(PSA) -- R/O Prostate Cancer Serum Creatinine MEDICATION THERAPY ALPHA-ADRENERGIC BLOCKERS • • Relax the smooth muscle of the bladder neck and prostate Improves urine flow Relax smooth muscle of the prostate BPH ALPHA-ADRENERGIC BLOCKERS Flomax- (tamsulosin) Cardura - (doxazosin) Hytrin – (terazosin) Uroxatral – (alfuzosin) Side effect orthostatic hypotension dizziness BPH 5 ALPHA-REDUCTASE INHIBITORS Decreases the size of the prostate gland Proscar (finasteride) Avodart – (dutasteride) Side effect *decreases libido, *erectile dysfunction BPH Minimally Invasive Therapy used when medication not effective relieves the manifestations of BPH less invasive than traditional surgery BPH Transuretheral Needle Ablation (TUNA) Low-wave radio frequency – to burn away a region of the enlarged prostate Improves the flow of urine 70% of pt. show marked improvement Little pain Early return to regular activities TUNA BPH Transuretheral Resection of the Prostate (TURP) Removal of inner prostate tissue Most common procedure Advantages 1. No external incision made 2. Shorter hospitalization 3. Complications – clot retention, hemorrhage, infection, catheter obstruction TURP CONTINOUS BLADDER IRRIGATION 3- way drainage system- useful in irrigating the bladder & preventing clot formation 3000 ml sterile normal saline Irrigation -- consist of continuous inflow & outflow of solution & drainage Maintain patency of catheter & tubing Urine drainage – light pink Blood clots are expected 1st 24-36hrs. after surgery CBI Catheter removal – assess amount, color and consistency of urine may experience burning on urination, dribbling is common BPH Complications Hemorrhage Obstructed catheter Urinary incontinence URINARY DIVERSIONS Procedure performed to divert urine from the bladder to a new exit site – STOMA Used to treat a. Cancer of the bladder b. Congenital anomalies c. Trauma to the bladder d. Neurogenic bladder URINARY DIVERSIONS 1. 2. 2 CATERGORIES Incontinent urinary diversion Continent urinary diversion URINARY DIVERSIONS INCONTINENT • • • DIVERSION Urine drains through an opening created in the abdominal wall An appliance is needed Most common – Ileal Conduit URINARY DIVERSIONS INCONTINENT • • • • DIVERSIONS – ileal conduit Ureters are excised from the bladder & resected to a part of the ileum Proximal end is sewn closed Distal end created to form a stoma Remaining intestinal segments – anatomosed URINARY DIVERSIONS INCONTINENT DIVERSIONS • Stents -- prevent occlusion from post-surgical edema Disadvantages: • Requires a external collection device • Visible stoma URINARY DIVERSIONS INCONTINENT DIVERSIONS Pre-op Management • Discuss social aspects of living with a stoma 1. Clothing 2. Changes in body image 3. Odor 4. Sexuality 5. Exercise URINARY DIVERSIONS INCONTINENT DIVERSIONS Post-op Management • Assess for complications a. Paralytic ileus/SBO • Make sure urinary stents are draining • U/O < 30cc/hr – dehydration/obstruction • Hematuria –1st 24-48 hours • Mucous threads in urine – normal occurrence URINARY DIVERSIONS Post-op • • • • • management (cont’d) Check stoma color– beefy red Increase fld. intake Empty pouch when 1/3 full/q2-3 hr. Meticulous skin care Avoid foods that give strong odor– cheese, eggs, asparagus URINARY DIVERSIONS CONTINENT • • • • • DIVERSIONS Intra-abdominal urinary reservoir Self catheterize every 4-6 hours No need external attachments Reservoirs constructed from different parts of the ileum/colon Kock, Indiana, Charleston pouch URINARY DIVERSION CONTINENT DIVERSIONS Post-op Management • Teach patient to catheterize pouch • Irrigate pouch • Adhere to strict catheterization schedule • Enterostomal therapy nurse QUESTION A patient returns to the unit following a TURP . His urinary drainage bag is filled with dark red fluid with obvious bloods clots. And he is having bladder spasms. What would you do first? a. Assess his intake/output since surgery b. Administer pain medication as ordered c. Report your assessment to the urologist d. Nothing, these are manifestations that are expected following a TURP QUESTION a. b. c. d. The nurse evaluates her teaching as effective when a patient with a newly continent ileal diversion is able to do which of the following? Demonstrate care for the collection device State the importance of reporting cloudy urine to the physician Demonstrate self-catherization of the stoma Identify factors that contribute to this condition Urinary Tract Cancers Prostate Cancer Cancer of the Bladder Cancer of the Prostate Most common cancer among men after skin cancer Highest incidence in AfricanAmerican men Risk Factors increases rapidly after age 50 Family history High intake of red meat and high fat dairy products Cancer of the Prostate Signs and Symptoms Often asymptomatic As malignancy enlarges, may have symptoms of urinary obstruction Blood in urine, semen and painful ejaculation may occur C/O back and hip pain, weight loss, anemia, oliguria may indicate metastases Cancer of the Prostate Assessment and Diagnosis Screening tools DRE PSA Normal: 0-4 ng/mL Transrectal Ultrasound (TRUS) Biopsy Cancer of the Prostate Treatment Surgical removal of the prostate TURP Laproscopic radical prostatectomy Radiation Teletherapy Brachytherapy Hormone Therapy Casodex DES Chemotherapy Cancer of the Bladder Most commonly seen in ages 50-70 Transitional-cell carcinoma of the bladder Papilillomatous growths in the bladder Risk factors Cigarette smoking (twice as much) Environmental carcinogens Frequent/recurrent bacterial infections History of urogenital cancers Cancer of the Bladder Assessment and Diagnosis Hematuria Bladder irritability Pelvic or back pain Diagnostic tests: Cystoscopy Ultrasound/CT Biopsies Cancer of the Bladder Treatment Transurethral Resection of Bladder Tumor (TURBT) Chemotherapy/Radiation BCG Methotrexate/5-FU/ vinblastin/Adriamycin Cystectomy Cancer of the Bladder Treatment Transurethral Resection of Bladder Tumor (TURBT) Chemotherapy/Radiation BCG Methotrexate/5-FU/ vinblastin/Adriamycin/cisplatin Cystectomy Partial Radical