Maxio - Perfint Healthcare
advertisement
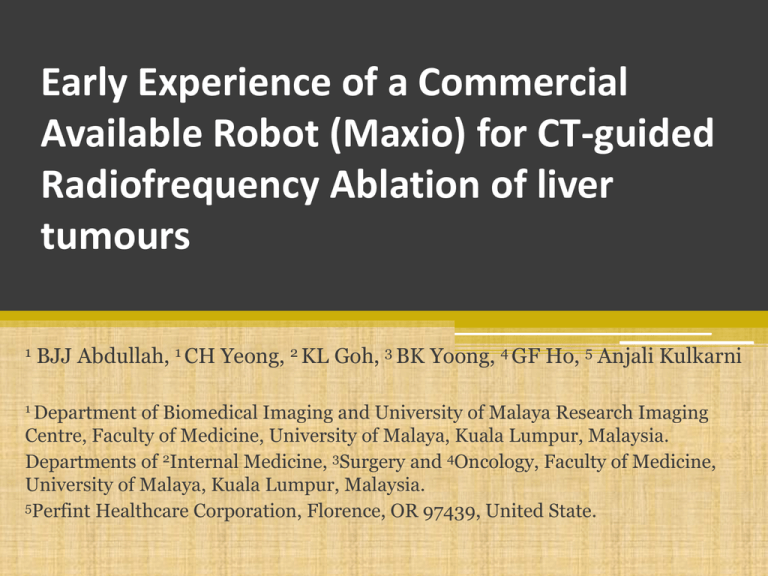
Early Experience of a Commercial Available Robot (Maxio) for CT-guided Radiofrequency Ablation of liver tumours 1 BJJ Abdullah, 1 CH Yeong, 2 KL Goh, 3 BK Yoong, 4 GF Ho, 5 Anjali Kulkarni 1 Department of Biomedical Imaging and University of Malaya Research Imaging Centre, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia. Departments of 2Internal Medicine, 3Surgery and 4Oncology, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia. 5Perfint Healthcare Corporation, Florence, OR 97439, United State. Challenges in Ablation Visualization Tumor visualization difficult in many cases Impossible to visualize related structures Skill dependent Positioning Needle visualization Complex spatial orientation of organs Multiple needle Big Learning Curve Local tumor progression occurs due to failures in establishing ablative margin (Minami & Kudo, 2011) Planning Limited Tools Current fusion techniques Cumbersome Ablation zone Validation No tool to validate Patient follow up Ablation tool lacks the critical level of control, accuracy, stability, and guaranteed performance (Emad M. Boctor et. Al, 2004) Challenges of current CT-guided RFA Real time Depth Entry point High CT fluoro dose Angle Target Repeated Punctures Time Consuming ECR 2014, Vienna 3 Robotic-Assisted RFA Integrated monitor (ROBIO EX-Console) MAXIO console MAXIO EX ROBIO Coordinate system Y Y X RS485 thro USB/ Serial to 485 converter to ROBIO console Z X CT Gantry Coordinate system Foot Switch om w ro e Revi l l wa CT Console Ethernet connection either thro hospital Network or thro a Ethernet Hub to CT MAXIOTM (Perfint Healthcare Pvt Ltd, Oregon, USA) ECR 2014, Vienna 4 Purpose of Study • To assess the accuracy of needle placement, radiation dose and performance level during robotic-assisted radiofrequency ablation (RARFA) of liver tumours using a CT-guidance robotic system (MAXIO, Perfint Healthcare, USA). ECR 2014, Vienna 5 Methodology • 19 patients (39 lesions, <5.0 cm diameter) were treated with RA-RFA. • All the procedures were performed under GA. • Following baseline CT scans the lesions were identified. • The CT images (1 mm reconstructed SL) were registered to the MAXIO workstation for treatment planning. • Target point (X, Y, Z) and needle entry point were determined during the treatment plan. • The needle trajectory path, angulation and depth of lesion were calculated and shown on the treatment plan. ECR 2014, Vienna 6 Methodology • The plan was carefully checked to avoid any critical organs or bone across the trajectory. • Once the plan was confirmed, MAXIO was executed. • The robotic arm then moved automatically to the planned location and the radiologist inserted the RFA needle through the bush holder at the end-effector of the robotic arm. • Post-needle insertion, a CT-fluoro was done to confirm accurate placement of the needle within the target volume. ECR 2014, Vienna 7 Methodology • The accuracy of needle placement, number of readjustments and total radiation dose to each patient were recorded. • The performance level was evaluated for each procedure on a five-point scale (5-1: Excellent-Poor) by the operated radiologist. • The radiation doses and readjustments were then compared against 30 RFA patients treated without robotic assistance. ECR 2014, Vienna 8 Image Registration Segmentation SCAN PLAN Simulation VISUALISE Adaptive Intra-op. registration EXECUTE VALIDATE MaxioTM ECR 2014, Vienna Post procedure confirmation Robotic Targeting 9 ECR 2014, Vienna 10 ECR 2014, Vienna 11 Results • All 39 lesions were targeted successfully. • No immediate complications were noted in all the patients. RA-RFA Average number of needle readjustment 0.8 ± 0.8 Performance level 4.7 ± 0.5 Conventional RFA P-value CT Fluoro Dose per Lesion 422.27 ± 370.611 (DLP, mGy.cm) (-16%) 501.20 ± 366.54 P>0.05 Total CTDIvol per patient (mGy) 534.71 ± 397.74 (-6%) 567.33 ± 398.62 P>0.05 Total DLP per patient (mGy.cm) 1390.37 ± 549.02 (-14%) 1611.27 ± 708.38 P>0.05 ECR 2014, Vienna. 12 Conclusion • Robotic-assisted planning and needle placement appears to be ▫ ▫ ▫ ▫ technically easier requires fewer number of needle passes fewer check scans lower radiation dose (patient & staff) • Study with large sample size is needed to confirm these preliminary findings. ECR 2014, Vienna 13 Other Potential Advantages of RA-RFA • Time • Pain • Allows access to difficult lesions • Accuracy & consistency • Level of confidence & safety ECR 2014, Vienna 14 References • BJJ Abdullah, CH Yeong, KL Goh, BK Yoong, GF Ho, Carolyn Yim, Anjali Kulkarni. Robotic-assisted radiofrequency ablation of primary and secondary tumours. European Radiology, Vol 23(9), 2013. • Perfint Healthcare Corporation official website. www.perfinthealthcare.com ECR 2014, Vienna 15