Radiofrequency Ablation of Lung Cancer
advertisement
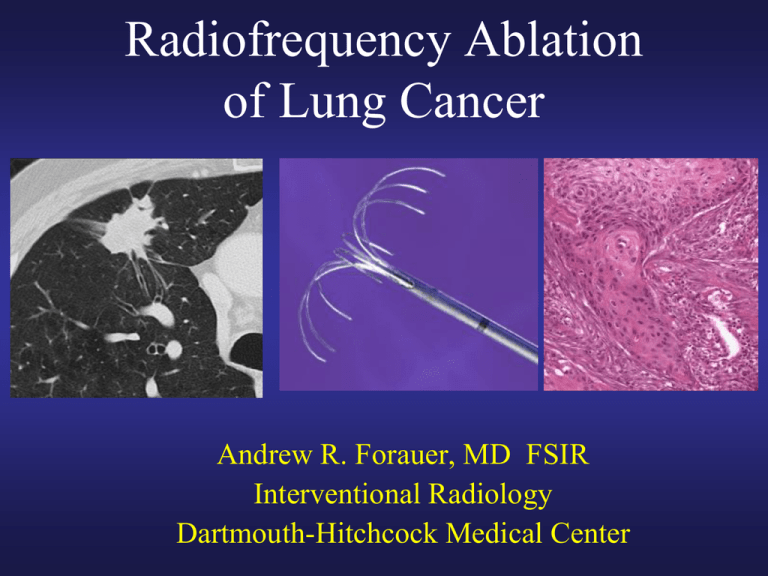
Radiofrequency Ablation of Lung Cancer Andrew R. Forauer, MD FSIR Interventional Radiology Dartmouth-Hitchcock Medical Center I have no financial disclosures (but am willing to entertain offers…) Modern Cancer Therapy Chemotherapy Radiation Therapy Surgery • Interventional Radiology is emerging as a fundamental discipline involved in cancer treatment • Percutaneous ablation • Embolization techniques • Intra-arterial drug delivery Radiofrequency Ablation (RFA) • Thermal (heat) based tumor ablation system • Most common clinical applications: – Liver – Kidney – Bone, other soft tissue Mechanism of action Thermal energy damage to cellular proteins, enzymes, & nucleic acids Creates a volume of tissue necrosis & coagulation Patient selection • Early stage patients who are good surgical candidates proceed to surgical resection • What about those with multiple co-morbidities and/or poor lung function? • Up to 50% of their mortality will still be Ca-related Tumor selection • • • • Solitary lesions (usually) 3 cm or less Non-small cell histology Location – Safe & reasonable percutaneous route – No extension to hilum/mediastinum – Not contiguous with major vessels or nerves Surgery Ablation Radiation Therapy RFA vs Surgical Resection Image-guided Ablation Surgical Resection • Well tolerated, no incision • Higher patient impact • Reliance on post-ablation imaging • Pathology available for margins • No assessment of nodes • Nodal status determined Sublobar resection, RFA, & cryoablation compared • Overall 3-year survival: – 87% (SLR), 87% (RFA), 77% (cryo) * • 3-year disease free survival: – 61% (SLR), 50% (RFA), 47% (cryo) * * No significant difference between the 3 groups Zemlyak et al., J Am Coll Surg, 2010 RFA vs External Beam Radiation Image-guided Ablation Radiation Therapy • Local therapy with less “collateral damage” • Effects on adjacent lung tissue & dosage limitations • Single session, but repeatable • Multiple visits • Fewer complications • Potential for procedural complications Radiation therapy (conventional EB) Surgical resection (LR, sub LR, VATS) No difference in DFS OS at 5 years: 40-55% Ablation ? OS at 5 years: 15-30% SBRT: Better at local dz control; OS @ 5 yrs ~50% RFA outcomes Overall survival data in RFA series tends to reflect a population with more co-morbidities, but Ca specific survival is encouraging Overall survival¹ Ca specific survival1,2 1 yr 70% 92% 2 yr 48% 73% 1. Lencioni R et al. Lancet-Oncol, 2008; 9:621-628 2. Zemlyak et al., J Am Coll Surg, 2010 3 yr -50% What about RFA and pulmonary metastases? RFA of lung metastases Study n Mean size 1-yr 2-yr OS OS 3-yr OS 5-yr OS Gillams ‘13 CVIR 122 1.7 cm (.5 – 4) 95% 75% 57% --- Chua ‘10 Ann. Oncol 148 4 cm (+/- 1.0) --- --- 60% 45% Yan ‘07 J Surg Oncol 30 - - - 75% 63% 45% Hiraki ‘07 JVIR 27 1.5 cm (.3 – 3.5) 96% 54% 48% Variety of histologies (~65% CRC) Hepatic dz at time of RFA 70 yr old patient w/ colorectal Ca & a LLL metastasis Pre-ablation CT Peri-procedural CT during probe positioning 4 month follow-up PET/CT; CEA now wnl Summary • RFA can be used to treat both primary & metastatic tumors • Doesn’t preclude other complimentary therapies • Patient selection is key/critical (not about the specialty, ego, or absolutes- its about the PATIENT) Current areas under investigation in IR • Chemotherapy delivered via the pulmonary artery • Selective chemoembolization • Combining chemotherapy infusions with ablation procedures Thank you for your attention !