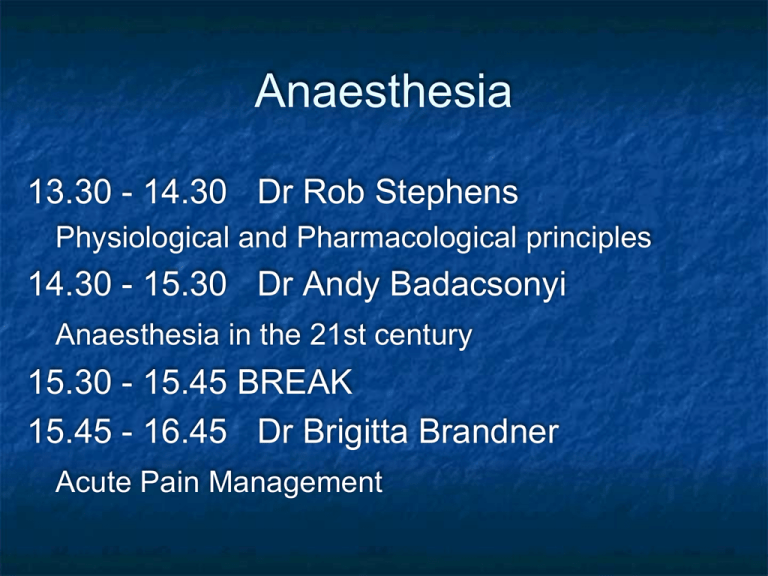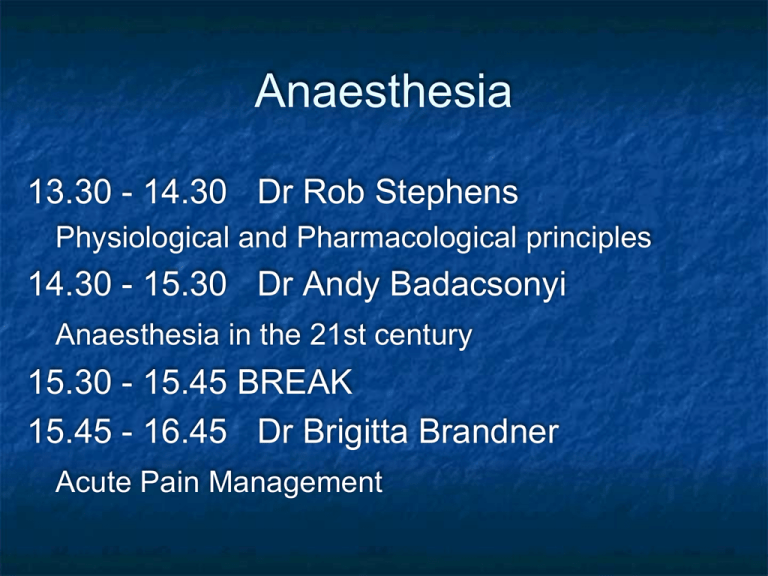
Anaesthesia
13.30 - 14.30 Dr Rob Stephens
Physiological and Pharmacological principles
14.30 - 15.30 Dr Andy Badacsonyi
Anaesthesia in the 21st century
15.30 - 15.45 BREAK
15.45 - 16.45 Dr Brigitta Brandner
Acute Pain Management
Physiology and …
Dr Rob Stephens
Thanks to Drs James Holding and Maryam Jadidi
Contents
Introduction
Physiology
CVS, RS, NS, Other
Pharmacolgy
Anaesthetic/ Hypnotic Agents
Neuromuscular Paralysis & Reversal
Analgesia
Others, CVS, Gasses, Fluids
Introduction
General word:
website, documents, coming to theatre
Introduction
Anaesthesia is more than Physiology and
Pharmacology!
Surgery vs Anaesthesia
Outside theatre
CVS physiology
O2 + C6H12O6
CO2 + H2O
ATP
O2 delivery
=Amount of O2 to tissues per minute
=Cardiac Output x O2 content of blood x
HR x SV
Hb x Sa02 x constant
CVS physiology
MAP = CO x SVR
HR x SV
Vaso-? constricted ? dilated
AT REST
5 l/min
RIGHT
HEART
L
H
100%
CVS physiology: Heart
Heart
pumps blood (02) from lungs to tissues
then back to heart / lungs (C013-15%
2)
rate
pre / afterload
contractility
7%
4-5%
Work =02 needs
Heart
Brain 9%
Gastrointestinal
20-25%
Kidneys
20%
15-20%
Muscles
Anaesthesia and CVS
CVS effects..
Anxiety, illness, walking to theatre, pain
Induction of general anaesthesia
or onset of epidural/ spinal anaesthesia
Cardiovascular - active drugs
Intubation
Surgical stimulation / trauma
Haemorrhage
Extubation
?Recovery or complication
Cardiovascular changes
‘artists impression’ version often filled in!
Preopera
tive
Induction of anaesthesia
Incision
Surgical stimulation
Cardiovascular Bleeding
Less oxygen in blood
Less pressure at Atrial and Aortic stretch
Sympathetic ++ response (+renal, adrenal)
Blood pressure maintained …
↑ CO x ↑ SVR
↑HR x ↑SV
vasocontricts
+ve inotrope
+ve chronotrope
vasocontricts
Respiratory
Upper – Airway
Lower- Trachea, lungs, muscles
Respiratory- Airway
Anaesthesia ‘Obtunds’ airway
=“Airway obstruction’
= no airflow
= no 02
= Badness
Respiratory- Airway
Keep Airway open:
Airway manoeuvres (chin lift etc)
Airway devices- above vs blow cords
Above
Vocal Cords
eg , gudel, LMA
Below Vocal Cords - Into trachea =
intubation, paralysis
Guedel / Oro-Pharyngeal
size 4
size 3
Adult male
Adult
female
Guedel
Laryngeal Mask Airway
Respiratory- Airway
Respiratory- Lower/ Lungs
Spontaneous vs Ventilated
Lungs smaller depth
Drugs respiratory rate
Small airways / Alveolar collapse
Can’t cough – secretions
= ‘pulmonary shunt (vs deadspace)
Hypoxaemia, persists postoperatively
CT scan of Diaphragm during
awake spontaneous breathing
CT scan of Diaphragm during
anaesthesia: Atelectasis
Gastrointestinal
General Anaesthesia
relaxes gastro-oesophageal sphincter
Fluid up oesophagus
?into lungs
starvation
postoperative vomiting
Other drugs (eg analgesia)
Neurology
Many Effects
GA
drug induced
reversable
unconsciousness
Many reflexes (airway, gag, CN)
Awareness
+/- NMJ paralysis
Physiology
2(3) factors determining blood pressure
How does GA affect these?
3 words about GA on resp system
Contents
Introduction – the classical triad
Introduction – general principles
Hypnotic Agents
Neuromuscular Paralysis + Reversal
Analgesia
Cardiovascular Drugs – up and down
Fluids and Gasses are drugs too!
Pharmacology Introduction
Anaesthesia ‘classical triad’
Hypnotic agent- unconsciousness
Gas or IV
Analgesia
Neuromuscular Paralysis
Induction, Maintenance, Emergence,
Recovery
Basics of anaesthesia: diagrams, handout &
lecture
Introduction - Principles
Pharmacokinetics
What the body does to the drug
Absorption, distribution, metabolism, elimination
Pharmacodynamics
What the drug does to the body – ie it’s effects
CVS, RS, GI, NS, Other , Side effects
Typical Anaesthesia
Intravenous induction Propofol
Short acting opiate - e.g. fentanyl
Hypnotic ‘anaesthetic’ - e.g. propofol
Set up of anaesthetic maintenance - e.g.
sevoflurane vapour in oxygen and air
Specific muscle paralysis may be needed
Definitive analgesia
Anti-emetic
Others
Hypnosis: Propofol
Hypnosis: Propofol (and others)
IV
Redistributed out of CNS
metabolised
CVS - CO x SVR = MAP
RS airway and lungs
NS pain on injection
Maintenance: Volatiles
Oxygen
Air
Sevoflurane
Maintenance
Sevoflurane (‘SEVO’)
Used for gaseous induction.
Desflurane
Isoflurane
CO x SVR = MAP
Gases, inhaled, little metabolised, exhaled
CVS: CO x SVR = MAP
RS- irritant, bronchodilate NS
Given with Oxygen /Air /Nitrous Oxide
MAC = minimum alveolar concentration
Muscle Paralysis
Neuromuscular blockers
Depolarising
Suxamethonium
Non-depolarising
Atracurium
Vecuronium
Rocuronium
Neuromuscular blockers
Depolarising
Suxamethonium 2x Ach molecules
Activates receptor
Non-depolarising – competitive vs ACh
Atracurium
Vecuronium
Rocuronium
Nicotinic ACh Receptor
Reversal of Paralysis
Neostigmine
Blocks cholinesterase
Stimulates nicotinic and
muscarinic
Given with an
anticholinergic
Sugammadex
Analgesia – Dr B
Systemic
Simple- paracetamol 1g
NSAID – Diclofenac etc
Opioids eg morphine 2mg bolus
Others – Ketamine
Regional – spinal / epidural / blocks
Local - infiltration
Uppers
Anticholinergics
Atropine
Glycopyrulate 200-600μg
Symatheto-mimetics
1 agonists
Phenylepherine
Metaraminol 0.25-0.5 mg
Ephedrine
mixed and adreno agonist
MAP = 1
1 2
CO x SVR
Downers
More anaesthetic or opiate / analgesia
Short acting -blockers (labetalol, esmolol)
Short acting blockers
GTN
MAP =
CO x SVR
Clonidine - 2 agonist clonidine
Antiemetics
Antiemetics
General- Hydrate, anxiety, gastric decompress
Cyclizine
anti-histamine
Ondansatron 5-HT3 receptor antagonists
S/E – constipation + long QT
Prochlorperazine (‘Stematil’) –
DA and mACh receptor antagonist
S/E – tachycardia and other anti-cholinergic effects
S/E – extrapyramidal
Dexamethasone glucocorticoid
S/E – deranged glucose control
Fluids and Gasses are drugs too!
Oxygen is a ‘drug’
Intravenous fluids
Colloids
Crystalloids
Blood and products
Articles on website / youtube
General Advice
Can always give more – can’t take away
Caution in
Unwell
Elderly
Hypovolaemic
Lots of ways to anaesthetise- don’t worry