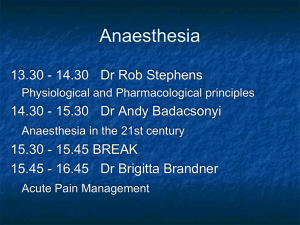
Anaesthesia for medical students! What does it mean?
advertisement

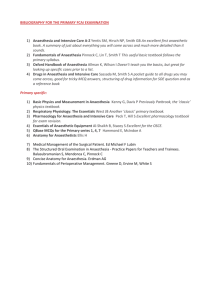
Anaesthesia for medical students! What does it mean? from Greek an-, "not/without" and aesthētos, "perceptible/ able to feel". Anaesthetists- the largest hospital speciality Anaesthesia for surgery Research (physiology, altitude, basic science etc) Resuscitation Transport of ill patients Management Intensive care Pain relief ‘Hospital at night teams’ Education Drugs in Anaesthesia The ‘Triad of anaesthesia’- a convenient way of thinking about anaesthetic drugs A person having an anaesthetic will often have a combination from 1 each. Consider CVS RS (airway / gas exchange) GI (reflux) NEURO METABOLIC effects 1 Hypnosis = unconsciousness Intravenous Propofol / Thiopentone / Etomidate / Methohexitone vs Ketamine Effect all organ systems to differing extents CVS – hypotension / dyrhythmias RS – Airway reflexes / respiratory depression (apnoea) GI - oesophageal sphincter tone (regurgitation) One off dose.. or infusions Sedation vs anaesthesia Metabolised by liver Elderly, ill, hypovolaemic need less – greater side effects (eg cardiac arrest) Ketamine – CVS stimulant, analgesia Gaseous- volatile =…….ane’ ‘Halothane’- (rarely used UK) Isoflurane / sevoflurane /desflurane / Enflurane Given (1-8%) with Oxygen (30%+) in air or Nitrous oxide Exhaled unmetabolised (80-99.4%) Action to cause hypnosis…?? Effect most organ systems CVS – hypotension / dysrhythmias RS – Airway reflexes / respiratory depression Can trigger Malignant hyperpyrexia 2 Analgeisa: WHO cancer analgesia ladder Simple eg paracetamol NSAIDS eg diclofenac/ ibuprofen Opiods quick (eg fentanyl, alfentanil, remifentanil) vs slow/long (eg dia/morphine) vs weak (eg Codeine Phosphate) + regional (eg nerve/root block) + central (spinal/epidural) + other eg N20, Tramadol, discussion, reassurance, splinting # 3 Paralysis: competitive vs non-competitive Normal Physiology: at NMJ, ACh released from nerves crosses cleft- ACh, Ca++ release Suxamethonium 30-60 secs on, 4-5 mins off, depolarises/non-competitive, enzymes degrade (cholinesterase) Vecuronium, atracurium, others etc longer onset minutes /offset 15-45mins: competitive either fall off as more ACh is made (naturally) or cholinesterase inhibitors Practicalities: the conduct of general anaesthesia Also has three parts… different problems.. different solutions 1 Induction – from consciousness to the ‘surgical plane’ of anaesthesia Either gaseous - slower, continuous respiration, not as nice(?) or intravenous - fast, may cause apnoea, greater CVS effects Airway very important during induction (competent cough/gag to absent) Quick CVS effects also potentially dangerous 2 Maintenance – during surgery Anaesthesia is CVS/RS depressant vs surgical stimulation Haemorrhage, surgical manipulation (eg vagal effect) all CVS depressant etc Can be gaseous or intravenous 3 Emergence – from anaesthesia to restoration of consciousness The opposite of induction; potentially dangerous time Airway important again Other effects (CVS, pain, Neurological etc) Practicalities: how to do it! Preoperative visit (Hx Ex Ix Discussion Plan) Anaesthetic room + surgery considerations Airway: secure/definitive vs non-secure Facemask, gudel airway, Laryngeal Mask Airway Endotrachel tube (COETT), Tracheostomy Breathing: spontaneous vs artificial ventilation (IPPV) Which volatile/ carrier gas / breathing system / ventilator / paralysis Circulation: IV Access / monitoring / fluids / drugs / blood Drugs: emergency and other Equipment: checked and appropriate? Analgesia: systemic (what, how much, when) vs regional Position and protection: supine/ side or prone; head down etc warmers, pressure areas etc Postoperative Where should the patient go? (ward/HDU/ICU/other hospital) Analgesia Monitoring and observations DVT prophylaxis Fluid Oxygen Communication (surgeon, nurses, patient, relatives) Could I have done anything different/better?