Bacillary Dysentery (shigellosis)
advertisement

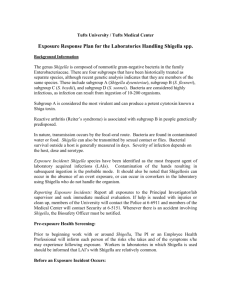
INTRODUCTION Acute infectious disease of intestine caused by dysentery bacilli Place of lesion: sigmoid & rectum Shigellosis is endemic throughout the world where it is held responsible for some 120 million cases of severe dysentery with blood and mucus in the stools EPIDEMIOLOGY About 1.1 million people are estimated to die from Shigella infection each year, with 60% of the deaths occurring in children under 5 years of age. about 500 000 cases of shigellosis are reported each year among military personnel and travellers from industrialized countries Since the late 1960s, pandemic waves of Shigella dysentery have hit sub-Saharan Africa, Central America and South and South-East Asia. AETIOLOGY Causative organism: dysentery bacilli, genus shigella, gram-stain negative, short rod,non-motile Groups: 4 groups & 50 serotypes - S. Dysenteriae-the most severe - S. Flexnerii- endemic in developing countries. easily turn to chronic - S. Boydii - S. sonnei -the most mild NORMAL HABITAT Found only in the human intestinal tract. Carriers of the pathogenic strain can excrete the organisms up to 2 wks after the infection &occasionally for longer periods. Killed by drying TRANSMISSION Transmitted by fecal-oral route High incidence of shigellosis occur in areas of poor sanitation and where water supplies are polluted. Lack of personal hygiene Young children are more frequently affected than adults [> 6 months] Horseflies are also thought to be important in transferring Shigella from faeces to food. Epidemics can be caused by ingestion of contaminated milk and milk products. Antigenic structure Differentiation into groups (A, B, C, and D) is based on O antigen serotyping; K antigens may interfere with serotyping, but are heat labile. Virulence factors toxin – An A-B toxin produced by S. dysenteriae and in smaller amounts by S. flexneri and S. sonnei. Enterotoxic, neurotoxic and cytotoxic effects Shiga This Damages intestinal epithelium and glomerular endothelial cells (associated with HUS) plays a role in the ulceration of the intestinal mucosa. OUTER MEMBRANE AND SECRETED PROTEINS These proteins are expressed at body temperature and upon contact with M cells in the intestinal mucosa they induce phagocytosis of the bacteria into vacuoles Shigella destroy the vacuoles to escape into the cytoplasm From there they spread laterally (Polymerization of actin filaments propels them through the cytoplasm.) to epithelial cells where they multiply but do not usually disseminate beyond the epithelium. SHIGA TOXIN ENTEROTOXIC EFFECT: Adheres to small intestine receptors Blocks absorption (uptake) of electrolytes, glucose, and amino acids from the intestinal lumen Note: This contrasts with the effects of cholera toxin (Vibrio cholerae) and labile toxin (LT) of enterotoxigenic E. coli (ETEC) which act by blocking absorption of Na+, but also cause hypersecretion of water and ions of Cl-, K+ (low potassium = hypokalemia), and HCO3- (loss of bicarbonate buffering capacity leads to metabolic acidosis) out of the intestine and into the lumen CYTOTOXIC EFFECT: B subunit of Shiga toxin binds host cell glycolipid A domain is internalized via receptor-mediated endocytosis (coated pits) Causes irreversible inactivation of the 60S ribosomal subunit, thereby causing: Inhibition of protein synthesis Cell death Microvasculature damage to the intestine Hemorrhage (blood & fecal leukocytes in stool) Neurotoxic Effect: Fever, abdominal cramping are considered signs of neurotoxicity PATHOGENESIS AND IMMUNITY Shigellosis is primarily a pediatric disease, and is restricted to the GI tract. Mean infective dose: 103. Mouth colon invade M cells and subsequently spread to mucosal epithelial cells cause microabscess in the wall of colon and terminal ileum necrosis of the mucous membrane, superficial ulceration, bleeding, and formation of pseudomembrane. INVASION OF INTESTINAL WALL BY SHIGELLA SHIGELLOSIS Two-stage disease: Early stage: Watery diarrhea attributed to the enterotoxic activity of Shiga toxin following ingestion and noninvasive colonization, multiplication, and production of enterotoxin in the small intestine Fever attributed to neurotoxic activity of toxin Second stage: Adherence to and tissue invasion of large intestine with typical symptoms of dysentery Cytotoxic activity of Shiga toxin increases severity CLINICAL DISEASE: ACUTE DYSENTERY Common Type Incubation period: 1-3 days Sudden onset of abdominal pain, fever and watery diarrhea, number of stools increase, less liquid, often contain mucus and blood, rectal spasms with resulting lower abdominal pain (tenesmus) symptoms subside spontaneously in 2-5 days in adult cases, but loss of water and electrolytes frequently occur in children and the elderly. a small number of patients remain chronic carriers. Some cases are accompanied by hemolytic uremic syndrome (HUS), characterized by acute hemolysis, renal failure, uremia, and disseminated intravascular coagulation. Death can occur from circulatory collapse or kidney failure. Total WCC is raised with neutrophilia Infection with S. dysenteriae can lead to leukemoid reaction developing 5-10 days after infection caused by an endotoxin. S. sonnei is not very pathogenic, therefore infections are rarely serious. Acute dysentery mild type: caused by S. sonnei low fever or no fever Abdominal pain is mild stool mixed with mucus, without blood & pus diagnosis by isolation bacteria TOXIC TYPE: Abrupt onset, high fever, Temperature rise to 40oC Listlessness, lethargy, convulsion, coma. circulatory & respiratory collapse diarrhea mild or absent at beginning shock form: septic shock brain form: respiratory failure mixed form CHRONIC DYSENTERY Chronic dysentery: > 2 months Chronic delayed type: diarrhea long-time and repeated Chronic obscure type: acute history in 1 year, no symptoms, stool culture Pos. or sigmoidscopy Acute attack type: same as common acute dysentery LABORATORY DIAGNOSIS Blood picture: total WBC count increase, neutrophils increase Stool examination: direct microscopic exam.: WBC, RBC, pus cells bacteria culture: Sigmoidoscope: shallow ulcer, scar, polyps TREATMENT oral rehydration therapy, intravenous fluid replacement Antibiotic treatment: chloramphenicol, ceftriaxone, ciprofloxacine, tetracycline, and trimethoprimsulfamethoxazole. Drug resistance is common. Restoration of electrolytes Opiates and anti-diarrhoea medications should be avoided. PREVENTION AND CONTROL Humans are the only reservoir for shigellae. Transmission of shigellae: water, food, fingers, feces, and flies. Most cases occur in children under 10 years of age. Prevention and control of dysentery: 1. Sanitary control of water, food and milk; sewage disposal; and fly control. 2. Isolation of patients and disinfection of excreta. 3. Detection of subclinical cases and carriers.